Anxiety disorders are the most prevalent mental health conditions affecting children and adolescents globally.1 These disorders can appear as early as preschool age and often have significant negative impacts on a young person’s daily life. They can impair academic performance, career prospects and social life, and can lead to ongoing mental health challenges. NHMRC-funded researchers at Macquarie University and the University of Queensland played key roles in demonstrating the importance of early anxiety intervention. Their work has led to the development of highly effective treatment methods that are now in use internationally.
Origin
Anxiety is a part of every person’s experience, however when it significantly interferes with daily life – causing excessive worry and avoidance of places, people and events – then this may indicate the presence of an anxiety disorder.
Anxiety is the most common mental health condition faced by young people, affecting 5-10% of children and adolescents from pre-school to school-end. Not only does anxiety involve personal distress, but it can dramatically affect a young person’s future. Anxious young people are more likely to have reduced academic performance, miss school days and drop out of school early. They are more likely to be bullied, rejected by other children and have difficulties making friends. They are also more likely to have health concerns and doctor’s visits and are at increased risk of depression, substance use and suicide.
While the importance of childhood anxiety is now well understood within the behavioural sciences and psychiatry, until the mid-1980s the idea that children and adolescents might experience anxiety was barely discussed within the academic literature.
However, in 1989, University of Queensland clinical psychologist Ron Rapee – who was researching anxiety in adults – began a collaboration with Mark Dadds – who was investigating psychological issues in children. The initial result of this collaboration was their publication in 1991 of a review of the literature relating to anxiety disorders in children. This review revealed that the nature, development and treatment of anxiety disorders at this developmental stage was one of the most neglected areas of research in psychopathology.
Because untreated health problems in young people can lead to increasing and cumulative problems later in life, the discovery of the magnitude of anxiety disorders facing children was an immediate ‘call to action’ for Rapee. Developing approaches for the diagnosis, understanding, assessment and treatment of the major types of childhood anxiety disorders was to become the long-term focus of Rapee’s research.
Investment
Commencing in 1992, the research of Rapee and colleagues Dadds, Jennie Hudson, Jordana Bayer and Heidi Lyneham, was funded by a series of NHMRC grants.
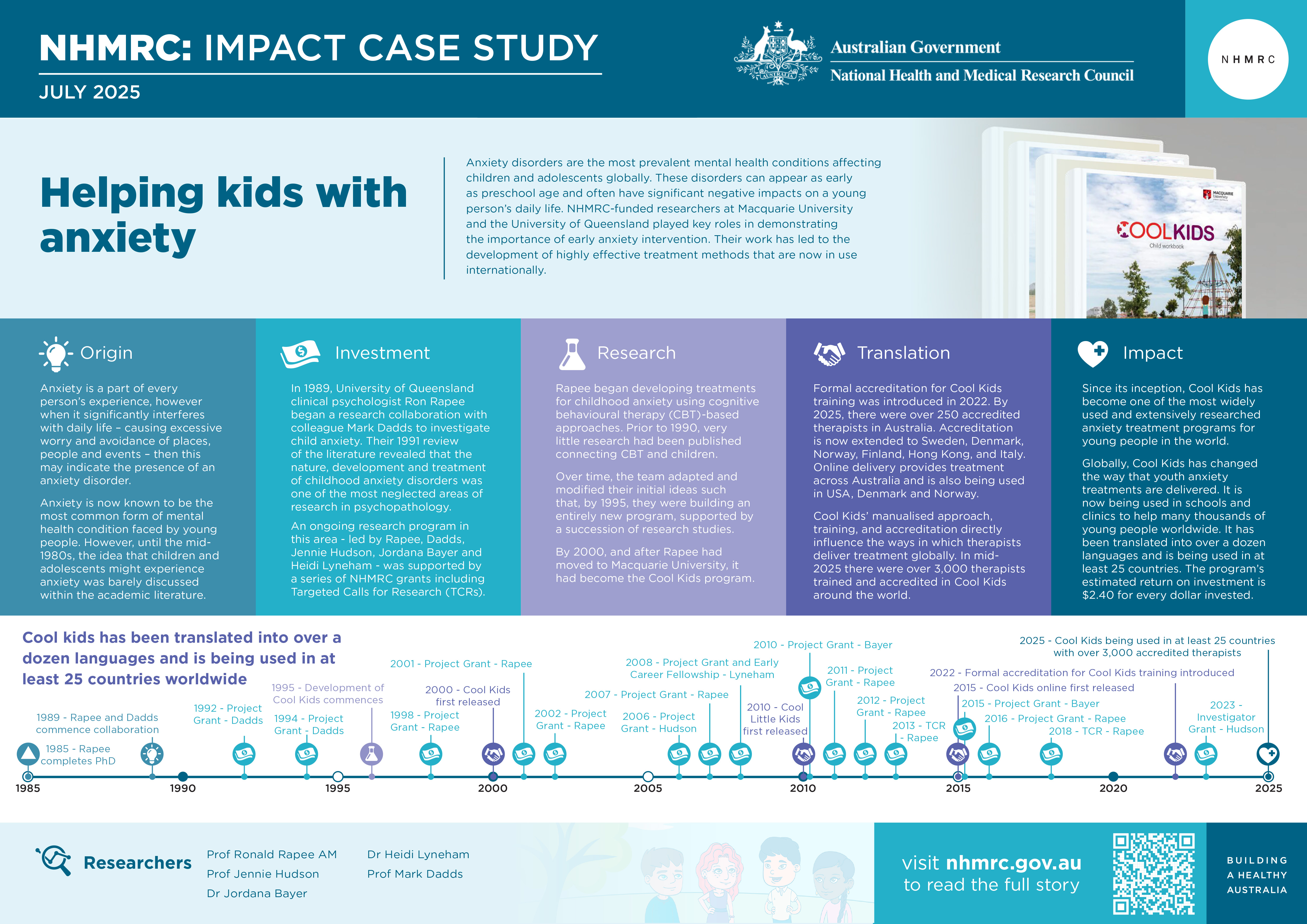
The PDF poster version of this case study includes a graphical timeline showing NHMRC grants provided and other events described in the case study.
Research
Rapee began developing treatments for childhood anxiety by seeking to both replicate and extend an effective approach based on cognitive behavioural therapy (or CBT), whose details had been published in the United States in 1994.2 Prior to 1990, very little research had been published connecting CBT and children.3
CBT is a type of psychotherapy that helps individuals manage their mental health concerns by identifying and changing unhealthy or negative thought patterns and behaviours. It is a goal-oriented therapeutic approach that focuses on the present and aims to improve quality of life by developing practical self-help strategies.
Over time, Rapee adapted and modified these initial ideas such that, by 1995, his team were building an entirely new program, underpinned by a succession of research studies. By 2000, and after Rapee had moved to Macquarie University, the program had become Cool Kids.
As it initially developed, Cool Kids aimed to teach children and adolescents (aged 7-17 years), and their caregivers, practical skills to help manage high levels of anxiety. Cool Kids is typically delivered to the family through a trained and accredited therapist. The program is supported by evidence-based, clear and detailed manuals for the therapist, caregiver and the young person. The standard program involves 10 sessions in clinic over 12 weeks.
About 60% of people who finish the program no longer meet the criteria for their original anxiety diagnosis by the end of treatment. This improves to 75% in the months that follow.
Extensive scientific evaluation has shown that the program also reduces depression, improves performance at school and relationships with friends and family. Not only are participants less distressed but so too are their families.
Over time, a variety of additional components to the program have been developed leading to versions for three different age groups: Cool Little Kids (3-6 years), Cool Kids (7–12 years) and Cool Kids (Chilled) (12-17 years).
Cool Little Kids has been used primarily as a program to prevent the development of anxiety and related problems in high-risk children. It is one of the few programs in the world to prevent anxiety that focus on underlying risk factors and has demonstrated prevention of anxiety and depression into mid-adolescence.4
Variations of the Cool Kids program have also been developed for young people who experience anxiety and severe depression, who are on the autism spectrum, who are being chronically bullied, or who have sleep difficulties or unexplained medical symptoms. There is also a version that can be delivered in schools.
Cool Kids can be delivered online and this provides help to young people who are unable to personally get to a therapist, including those who live in rural and remote regions. Through Cool Kids online, young people and their parents can access lessons through a dedicated website and they can also receive help from a therapist through regular phone calls.

In developing and extending Cool Kids, Rapee and his team have collaborated extensively with international teams (e.g. in Denmark, USA, Norway and Finland) who have sought to evaluate the application of Cool Kids and related programs in their own countries. The Australian team has collaborated with researchers in countries such as Vietnam and Turkey, as part of an innovative project to treat youth in low-income countries
Additional collaboration with the UK has explored the idea that a participant’s genes can impact their treatment. This work has identified a range of risk factors and has guided the development of new targeted interventions. The team has also conducted the first empirical trial of anxiety treatment within autism, changing the way that people on the autism spectrum receive treatment. This has led to extensive international research.
Translation
Formal accreditation for Cool Kids training was introduced in 2022. By 2025, there were over 250 accredited therapists in Australia. Accreditation is now extending to Sweden, Denmark, Norway, Finland, Hong Kong, and Italy.
Online delivery not only provides treatment across Australia but is also being used in USA, Denmark and Norway. Cool Kids’ manualised approach, training and accreditation directly influence the ways in which therapists deliver treatment globally. In mid-2025 there were over 3,000 therapists around the world trained and accredited in Cool Kids.
Cool Kids has influenced health services in Australia. The Australian Productivity Commission used Cool Little Kids as a case study to recommend the benefits of early intervention using online mental health treatment programs.5 Cool Kids has also influenced health services overseas. It has been listed in health guidelines, officially endorsed by the Danish and Slovenian governments, and is being considered by the Canadian Government as its primary youth anxiety program.
Outcomes and impacts
When Rapee and his colleagues began working in the field of child anxiety disorders, this problem was almost unrecognised internationally, despite it now being recognised as the most common form of mental health condition across all age groups. Their research has strongly influenced ways in which youth anxiety is identified, understood and treated, and it heralded international recognition of the significance of this issue among both professionals and the public.
Since its inception, the empirically validated Cool Kids program has grown to become one of the most widely used and extensively researched anxiety treatment programs for young people in the world. Cool Kids online provides young people in some of the most remote regions of Australia with the help that they need, and globally, Cool Kids has changed the way that youth anxiety treatments are delivered. It is now being used in schools and clinics to help many thousands of young people worldwide. It has been translated into over a dozen languages (including Chinese, Turkish, Indonesian, Icelandic and Korean) and is being used in at least 25 countries, both developed and developing.
Modelling by the National Mental Health Commission has demonstrated that a trial 3-year implementation of the Cool Little Kids program would cost $3.7 million but lead to savings of $8.7 million, or a return on investment of $2.40 for every dollar invested.6
Researchers
Professor Ronald Rapee AM
Ronald Michael Rapee completed his PhD in 1985. He is now a Distinguished Professor in the School of Psychological Sciences, Macquarie University, Sydney. Rapee has received several awards for his scientific contributions, including the Distinguished Contribution to Science from the Australian Psychological Society. In 2012, Rapee was made a Member of the Order of Australia for service to clinical psychology as a leader in the research and development of treatment programs for anxiety disorders, particularly in children.
Professor Jennie Hudson
Jennie Hudson graduated from Macquarie University with a Bachelor of Arts (1995) then a PhD (1999) and a Master of Clinical Psychology (2001). Hudson is Director of Research at the Black Dog Institute and was previously Director of the Centre for Emotional Health at Macquarie University. During 2015-2020, Hudson was a Visiting Fellow at the University of Oxford.
Dr Jordana Bayer
Jordana Bayer completed psychology at The University of Adelaide and then (in 1994) a Master of Clinical Psychology at Flinders University in South Australia. As a registered clinical psychologist she was employed at Flinders Medical Centre (Child Protection Service) before relocating to Melbourne in 1996. Bayer completed her PhD at the University of Melbourne in 2003 then undertook postdoctoral research at the Murdoch Children’s Research Institute and Royal Children's Hospital, Melbourne. Bayer is currently Adjunct Professor Advanced Practice at La Trobe University.
Dr Heidi Lyneham
Heidi Lyneham completed her PhD in 2004 and is currently Clinic Director at Macquarie University’s School of Psychological Sciences, within the Lifespan Health and Wellbeing Research Centre. Lyneham has worked within the Centre’s Emotional Health Clinic as a clinical psychologist and researcher for over 20 years.
Professor Mark Dadds
Mark R Dadds completed his PhD in 1986. He is a clinical psychologist who currently directs the Sydney Child Behaviour Research Clinic at the University of Sydney (USyd). He is also Professor of Psychology at USyd and is Director of Growing Minds Australia, a clinical trials network for child and adolescent mental health supported by the Australian Government’s Medical Research Future Fund.
Other researchers
The impacts described in this case study are also the result of the work of Professor Maree Abbott, Dr Paula Barrett, Dr Anne Chalfant, Dr Mary-Lou Chatterton, Dr Michael Cunningham, Dr Susan Edwards, Professor Maria Kangas, Dr Susan Kennedy, Dr Lauren McLellan, Professor Cathy Mihalopoulous, Dr Amy Morgan, Dr Carolyn Schniering, Dr Lynn Sweeney, Dr Anne Wignall and Professor Viviana Wuthrich.
Professor Rapee would like to thank Professor Philip Kendall, Temple University, USA, for his generosity and support.
Partner
This case study was developed with input from Professor Ron Rapee and in partnership with Macquarie University.

References
The information and images from which NHMRC’s Impact Case Studies are produced may be obtained from a number of sources including our case study partner, NHMRC’s internal records and publicly available materials. Key sources of information consulted for this case study include:
1 Polanczyk GV, Salum GA, Sugaya LS, Caye A, & Rohde LA. (2015). Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Child Psychology and Psychiatry, 56(3), 345–365
2 Kendall PC. (1994). Treating anxiety disorders in children: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 62, 100-110.
3 Benjamin CL, Puleo CM, Settipani CA, Brodman DM, Edmunds JM, Cummings CM, Kendall PC. (2011). History of cognitive-behavioral therapy in youth. Child Adolesc Psychiatr Clin N Am. Apr;20(2):179-89
4 Rapee RM. (2013). The preventative effects of a brief, early intervention for preschool-aged children at risk for internalising: Follow-up into middle adolescence. Journal of Child Psychology and Psychiatry, 54(7), 780-788
5 Productivity Commission. (2020). Mental Health, Report no. 95 Australian Government.
https://www.pc.gov.au/inquiries/completed/mental-health/report
6 National Mental Health Commission. (2019). The economic case for investing in mental health prevention. Australian Government National Mental Health Commission. https://www.mentalhealthcommission.gov.au/sites/default/files/2024-03/the-economic-case-for-investing-in-mental-health-prevention---summary.pdf