In the 2000s, rising annual Human Immunodeficiency Virus (HIV) diagnoses in Australia highlighted the need for developing new ways of preventing HIV transmission. Researchers at the University of New South Wales’ (UNSW) Kirby Institute and the Centre for Social Research in Health conducted a series of NHMRC-supported studies demonstrating the effectiveness of antiretroviral medicines in preventing transmission. Their work guided the successful scale up of HIV treatment as prevention and pre-exposure prophylaxis (PrEP), resulting in substantial declines in HIV infections in Australia and ensuring Australia remains a global leader in HIV prevention.
Origin
HIV is a virus that attacks and weakens the immune system. If left untreated, it leads to a gradual decline in immune function, resulting in Acquired Immunodeficiency Syndrome (AIDS) which increases the individual's susceptibility to life-threatening opportunistic infections. HIV transmission occurs through specific bodily fluids, including in the context of sex, pregnancy, childbirth, breastfeeding (from mother to child), and needle sharing where blood-to-blood contact may occur. It is not transmitted via saliva (for example, kissing, spitting, sneezing, or coughing), or through insect bites.
Historically, public health campaigns aimed at reducing HIV transmission focused predominantly on promoting condom use during sexual activities and reducing needle sharing. While condom use remains highly effective in preventing HIV, inconsistencies with its usage means that long term effectiveness is less than 100% (estimated at 91%).1 This suboptimal protection necessitated the need for research into more effective prevention methods to combat HIV transmission.
In the late 2000s, breakthroughs in biomedical technologies with antiretroviral therapy (ART) and PrEP significantly advanced HIV prevention practices. HIV infection is measured by the amount of HIV virus in the blood, also known as the viral load. When an individual has a viral load of fewer than 200 copies per mL of blood, it is considered as suppressed or ‘undetectable’ as it falls below the detection threshold of commonly used HIV tests. This can be achieved through ART, which, while not a cure, prevents the virus from replicating, reducing the viral load and reversing immune system damage. ART enables people with HIV to live healthier and longer lives. However, studies validating the efficacy of ART in preventing HIV transmission predominately involved heterosexual couples, limiting their relevance to men who have sex with men (MSM) populations in Australia. In 2023, 85% of the estimated 30,010 people living with HIV in Australia were men, with 63% of new notifications occurring in MSM.2
Antiretrovirals also play a crucial role in the prevention of HIV transmission through PrEP, where individuals without HIV take regular antiretroviral medication to prevent infection. With optimal adherence, oral PrEP (emtricitabine/tenofovir) is over 99% effective at preventing sexual transmission of HIV.3 However, while the individual-level efficacy of PrEP had been proven in randomised controlled trials, global implementation of PrEP was insufficient and no effect had been observed at the population level.
Researchers at UNSW sought to address these important knowledge gaps by investigating the protective effect of undetectable viral loads achieved through ART in MSM, alongside PrEP's efficacy at the population level.
Investment
NHMRC’s Council first established a working party on AIDS in 1983. The working party was provided reports of confirmed and suspected AIDS cases in Australia from state authorities. Based on recommendations from the working party and Council, NHMRC funded research on AIDS through a special funding round of research grants starting in 1984. Since then, NHMRC has funded well over 600 projects focussing on HIV and AIDS.
Researchers at UNSW's Kirby Institute and the Centre for Social Research in Health, including Andrew Grulich, Benjamin Bavinton, Martin Holt, Rebecca Guy and Richard Gray were supported by NHMRC to conduct research in various HIV areas. These areas included:
- Treatment and prevention of sexually transmitted infections (STIs)
- Links between STIs and risk of HIV transmission
- Undiagnosed HIV, HIV testing, and HIV transmission
- Monitoring of HIV cases and HIV transmission
- Behavioural and biomedical HIV prevention and increasing the impact of different HIV prevention techniques.
The researchers also received funding for their work on preventing and monitoring HIV transmission from state and territory health departments, the United States National Institutes of Health, and the pharmaceutical industry.
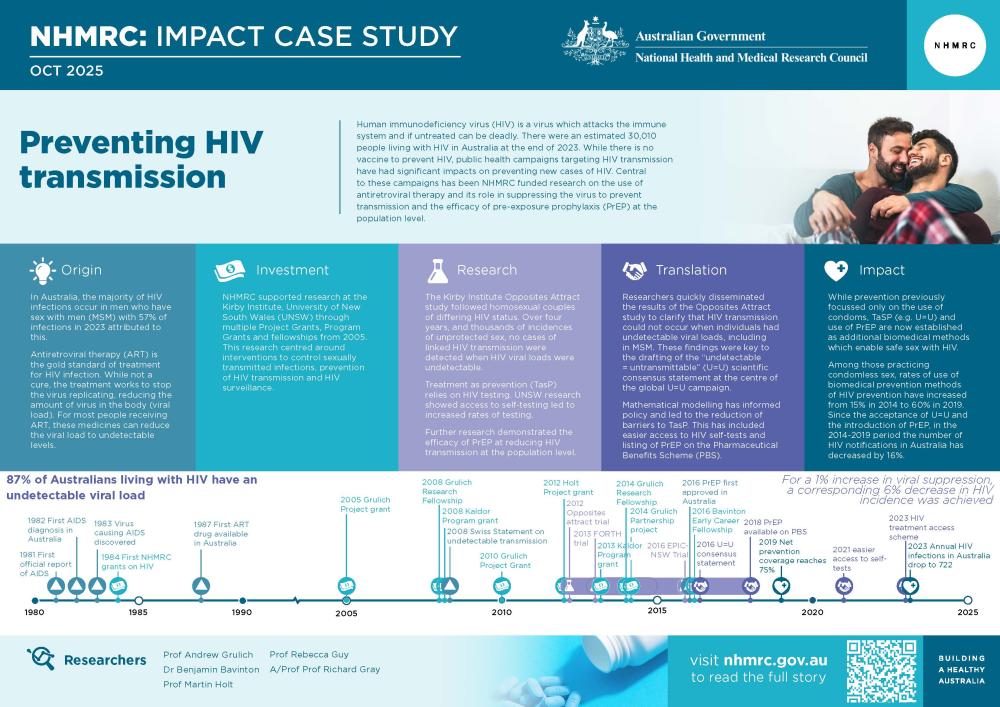
The PDF poster version of this case study includes a graphical timeline showing NHMRC grants provided and other events described in the case study.
Research
Treatment as prevention
In 2008, the Swiss National AIDS Commission released a statement indicating that an individual living with HIV on ART with an undetectable viral load could not transmit HIV. The HPTN (2011) and PARTNER (2014) studies,4,5 conducted by researchers from the University of North Carolina and University College London respectively, provided the first evidence that HIV treatment could be used to prevent HIV transmission (treatment as prevention – TasP). However, while these studies demonstrated the value of TasP, over 98% of the 2,600 couples involved in the studies were heterosexual. Consequently, the applicability of this vital information to MSM, who represent the majority of new notifications in Australia, was unknown.
UNSW researchers sought to address this important knowledge gap through an observational study examining whether undetectable viral loads achieved through ART provided protection from HIV transmission in MSM. Further, they examined whether the presence of other STIs, which they had previously shown to increase transmission of HIV,6 would influence transmission where viral loads were undetectable.
The Opposites Attract study followed 358 male homosexual serodiscordant couples (where one partner was HIV negative and the other HIV positive) in Australia, Brazil, and Thailand over 4 years (2012 to 2016).7 The study monitored instances of condomless anal intercourse and examined new cases of HIV infection in HIV negative partners. Across 12,447 instances of condomless sex where the HIV negative partner was not on PrEP and the HIV positive partner had an undetectable viral load, no cases of linked HIV transmission were detected. This was despite the prevalence of other STIs among participants. The PARTNER2 study (2019) independently corroborated these findings,8 showing no detection of HIV transmission from HIV positive individuals with undetectable viral loads in gay couples.
UNSW researchers conducted several behavioural studies and investigations into the extent to which TasP has affected population-level diagnoses in Australia, both within and outside of Opposites Attract. In partnership with community organisations and clinics, they also investigated the impact of TasP at a population-level. The NHMRC funded TAIPAN study, led by Associate Professor Denton Callander, established a retrospective cohort of more than 100,000 gay and bisexual men (GBM) across 2 states and showed there was a 66% reduction in HIV incidence during the period of TasP in 2010–2019, with the decline enhanced during a period of TasP and PrEP roll out.9
HIV self-testing
TasP relies strongly on a person being diagnosed with HIV and regular testing. In 2014, 9% of GBM with HIV were undiagnosed but accounted for the majority of new HIV infections in Australia.10 A key way to increase access to testing was shown to be through HIV-self testing in a person’s home, outside of clinical services, but when the technology first became available its potential use was controversial and policy shifts were needed nationally and globally.
In partnership with community organisations and clinics, researchers at UNSW conducted a waitlist randomised controlled trial (RCT) called FORTH from 2013 to 2015,11 funded by an NHMRC Program Grant. It showed that access to HIV self-testing resulted in an unprecedented increase in the frequency of testing among GBM, two-times overall and nearly four times in non-recent testers, without reducing the frequency of clinic-based HIV testing, and no adverse effects.
PrEP use/attitudes in Australia
UNSW researchers also undertook a number of studies and trials related to PrEP use and attitudes in Australia. Some of their earliest work demonstrated the case for PrEP, showing that GBM who had condomless sex, had STIs, or used drugs for sex were at higher risk of HIV.12
While the individual-level efficacy of PrEP had been proven in RCTs, implementation around the world was insufficient and no effect had been seen at the population level. From 2016 to 2018, UNSW researchers conducted the EPIC-NSW trial, where they commenced almost 10,000 GBM on PrEP. Their results showed that HIV diagnoses in New South Wales dropped by almost one-third after 2 years,13,14 demonstrating PrEP’s efficacy at the population level.
Translation
The Opposites Attract study, along with the HPTN and PARTNER studies, formed the evidence base for the first ‘Undetectable=Untransmissible’ (U=U) international Scientific Consensus Statement drafted in 2016.15 The statement asserts that there is effectively no risk of HIV transmission through condomless sex when a person living with HIV has a viral load that is suppressed/’undetectable’. Grulich, the Principal Investigator of the Opposites Attract study, was one of the four scientists who drafted this statement.
The U=U statement became key to the global U=U campaign promoting awareness of treatment as HIV prevention. During a conference in 2019, Dr. Anthony Fauci, then director of the National Institute of Allergy and Infectious Diseases, referred to the U=U discovery as 'the foundation of being able to end the epidemic'.
Results from the FORTH study also led to a paradigm shift in the way HIV testing was offered globally and propagated policy changes around the world. The RCT was one of only 5 studies globally which contributed to the evidence-base underpinning the first WHO guidelines on ‘HIV self-testing and partner notification guidelines 2016,16 and the WHO 'HIV self-testing strategic framework: A guide for planning, introducing and scaling up October 2018'.
In Australia, research by the UNSW team on the use, preferences, acceptability, and usability of HIV self-testing also led to national policy changes by the Therapeutic Goods Administration to ease limitations on the supply of HIV self-tests. From 2021, supply of HIV self-tests became easier through online purchases, over-the-counter sales in pharmacies, and to other relevant businesses, organisations and institutions that work with HIV at-risk communities including GBM.17
UNSW researchers conducted modelling work for submission to the Pharmaceutical Benefits Advisory Committee (PBAC) on the cost-effectiveness of HIV PrEP in Australia on behalf of the Australian Federation of AIDS Organizations (now Health Equity Matters). This work contributed to the listing of HIV PrEP onto the Pharmaceutical Benefits Scheme (PBS) and formed the basis for the Australasian Society for HIV Medicine (ASHM) PrEP guidelines.18,19 Following this, they continued to develop a range of ways to assess uptake and impact of biomedical prevention. They investigated GBM’s preferences for new types of PrEP and explored ways for reducing disparities in access to effective prevention methods (for example, engaging overseas-born GBM, younger men, and people who live outside of inner-city areas).20,21 Their research showed that PrEP was the most common prevention strategy used by GBM.22
Their research also identified that people born overseas are a priority population for the HIV response. Temporary residents living with HIV in Australia are ineligible for a Medicare card and hence, could not access subsidised ART through the PBS. Supported by NHMRC, the UNSW team developed and applied mathematical models of HIV transmission within Australia.23,24,25,26 Their results showed that providing ART to temporary residents would prevent infections and be cost-neutral to the Australian Government.27,28 This work contributed to the implementation of the HIV treatment access scheme program in 2023 by the Australian Government, which allowed people living with HIV who are ineligible for Medicare to access their treatment free of charge through government-funded hospital pharmacies.29
Outcomes and impacts
The multiple streams of research undertaken by UNSW researchers resulted in the adoption of U=U, TasP, PrEP and HIV self-testing into policies, programs and clinical practice guidelines both nationally and internationally.
Australian impacts
The research conducted by UNSW researchers resulted in greater use of effective HIV prevention methods and reduced HIV diagnoses in Australia. Their work has described how GBM in Australia are willing to rely on and use TasP in their sex lives, how TasP is negotiated and how effective TasP is in preventing HIV infections in Australia.8,30,31,32,33,34,35,36
Awareness of U=U has grown substantially in Australia, with 76% of GBM reporting that they knew about U=U by 2021.37 Higher levels of awareness and belief in U=U’s efficacy were observed among people living with HIV and PrEP users. The acceptance of U=U and the implementation of PrEP led to a 16% decrease in annual HIV notifications (which indicate the number of new HIV infections) between 2014 and 2019.38 Between 2010 and 2023, the prevalence of viral suppression in an Australian cohort of people living with HIV increased from 69% to 87%.8 Even adjusting for the use of PrEP, U=U led to significant reductions in HIV in GBM. With every 1% increase in viral suppression, a corresponding 6% decrease in HIV incidence was achieved.
There is now a national online HIV self-testing program led by Australia’s peak body for people living with HIV, and HIV self-testing is available in pharmacies and vending machines in the community. Individuals living with HIV, including those who are ineligible for Medicare, can access free ART treatment for their HIV. For those with Medicare, PrEP costs as little as 47 cents a day, with concession card holders able to access PrEP for about 8 cents a day. Individuals without Medicare access at risk of HIV transmission can access free oral PrEP. Newer technologies such as injectable PrEP are also becoming available to allow alternatives to daily oral PrEP.
While safe sex for prevention of HIV previously focussed only on use of condoms, treatment as prevention (U=U) and use of PrEP are now established as additional biomedical methods which enable safe sex that prevents HIV transmission. These 3 methods together are known as combination HIV prevention. Net prevention coverage, or the level of protection achieved in the community by the use of any of these combined HIV prevention methods, increased from 68% among GBM in 2014 to 75% in 2019.39 Among those practicing condomless sex, reliance on biomedical prevention increased from 15% in 2014 to 60% in 2019. Further, those who engage in condomless sex with no biomedical interventions appear to be less at risk than previously, including making decisions about which sexual partners to have, based on their partner’s viral load and use of PrEP.22
International impacts
The U=U Scientific Consensus Statement has since been endorsed by leading global HIV researchers and more than 1,000 organisations from over 100 countries, including WHO, UNAIDS, CDC, NIH, and hundreds of other HIV prevention organisations. U=U is a key message in advertising campaigns from not-for-profit organisations such as the National Association of People with HIV Australia and ACON (AIDS Council of NSW) in Australia, which are focussed on eliminating new HIV transmissions, spreading accurate information, and promoting inclusion. In 2024, Australia became the fourth country to endorse the ‘Multinational Undetectable = Untransmittable (U=U) Call-to-Action’, incorporating U=U into Australia’s efforts to prevent, diagnose, and treat HIV.
Internationally, in 2022, there were 29.8 million people living with HIV receiving ART, representing about 89% of people living with HIV who know their HIV status.40 Of those on ART, approximately 93% had suppressed viral loads. There is still a gap to reach the UNAIDS global target of 95% of people knowing their status among people living with HIV, 95% of those diagnosed on ART, and 95% of those on ART having suppressed viral loads. These targets, which were adopted by UN member states in 2001, focus on the identification of people living with HIV and preventing transmission through greater uptake of treatment.
UNSW researchers’ demonstration of how PrEP could be incorporated into global, national and state/territory HIV strategies has been reflected in the National HIV Strategy, UNAIDS’ 2020 Global AIDS Update, and WHO’s Consolidated Guidelines on HIV Prevention, Testing, and Treatment (2021).41 As a result of the FORTH study and other studies on self-testing, HIV-self-testing became a key tool to achieve equity in HIV control, and new policies have since been implemented widely with over 90 countries now supporting the sale of HIV self-tests. From 2018–2023, 42 million HIV self-tests were procured globally, with 133–283 million projected in 2022–2027.42 HIV self-testing is now used in programs in more than 70 countries to reach people at risk of HIV who face stigma, discrimination and other barriers to accessing HIV testing at clinical services.
Researchers
Scientia Professor Andrew Grulich
Andrew Grulich completed a Bachelor of Medicine and Bachelor of Surgery at the University of Adelaide in 1986 and a Master of Science in epidemiology at the London School of Hygiene & Tropical Medicine in 1990 before going on to complete his PhD at UNSW in 1998 on the epidemiology of HIV-associated cancer. He currently works as a researcher at the Kirby Institute, where he has been employed since 1995 and has worked in HIV research for more than 30 years. He is a member of the governing council of the International AIDS Society and a past president of the Australasian Society for HIV Medicine.
Associate Professor Benjamin Bavinton
Benjamin Bavinton completed a Bachelor of Arts Psychology (honours) at the University of Wollongong in 2003 and a Master of Public Health at UNSW in 2011 before completing his PhD at UNSW in 2017. He is currently an Associate Professor and Group Leader of the Biobehavioural Prevention Research Group within the HIV Epidemiology and Prevention Program at the Kirby Institute. Bavinton won two national awards for the Opposites Attract study: The 2019 Aileen Plant Memorial Prize for Infectious Diseases Epidemiology and the 2021 Sax Institute Research Action Award.
Professor Martin Holt
Martin Holt completed a Bachelor of Psychology (honours) at the University of Birmingham in 1996 and a Master of Science in social psychology at the London School of Economics and Political Science in 1997. He then went on to complete a PhD in psychology at the University of Birmingham in 2001. He has worked at the Centre for Social Research in Health at UNSW since 2003, where he leads the HIV research program, and is currently the Associate Dean, Research Quality & Culture in the Faculty of Arts, Design & Architecture, UNSW. Holt leads the GBQ+ Community Periodic Surveys which are the main part of Australia's behavioural surveillance system for HIV.
Scientia Professor Rebecca Guy
Rebecca Guy completed a Bachelor of Medical Science at University of Tasmania, a Masters of Epidemiology at ANU and PhD at Monash University in 2008. Guy is Head of the Surveillance Evaluation and Research Program at the Kirby Institute and also serves as a Member of the Institute’s Executive Committee and the Aboriginal and Torres Strait Islander Committee. She won the Gustav Nossal Medal for Global Health (2022) for her research on novel diagnostic strategies, including the FORTH HIV self-testing trial.
Associate Professor Richard Gray
Richard Gray completed a Bachelor of Science (honours) focused on Mathematics and Physics at UNSW. He then completed a PhD at the University of Sydney in 2007 in theoretical neuroscience. He has worked in the field of HIV and infectious disease modelling at the Kirby Institute and UNSW since 2007. Gray has performed modelling and evaluation studies for multiple organisations including the World Bank, World Health Organisation, UNAIDS, AusAID alongside national and international government bodies. He currently leads the Mathematical Epidemiology and Evaluation Research Group and is responsible for producing annual estimates of the Australian HIV cascade.
Partners
This case study was developed with input from Andrew Grulich, Benjamin Bavinton, Martin Holt, Rebecca Guy and Richard Gray in partnership with the Kirby Institute and UNSW.

References
The information and images from which impact case studies are produced may be obtained from a number of sources including our case study partner, NHMRC’s internal records and publicly available materials. Key sources of information consulted for this case study include:
1 Johnson WD, O’Leary A, Flores SA. Per-partner condom effectiveness against HIV for men who have sex with men. Aids. 2018 Jul 17;32(11):1499-505.
2 King, J., Kwon J., McManus, H., Gray, R., & McGregor, S., 2024, HIV, viral hepatitis and sexually transmissible infections in Australia: Annual surveillance report 2024, The Kirby Institute, UNSW Sydney, Sydney, Australia.
3 Centers for Disease Control and Prevention. Clinicians’ Quick Guide: What Is Oral HIV PrEP?. 2022 [cited 2024 Dec 9]. https://www.cdc.gov/hivnexus/prevention-brochure
4 Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Hakim JG, Kumwenda J, Grinsztejn B, Pilotto JH, Godbole SV. Prevention of HIV-1 infection with early antiretroviral therapy. New England journal of medicine. 2011 Aug 11;365(6):493-505.
5 Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, Van Lunzen J, Corbelli GM, Estrada V, Geretti AM, Beloukas A, Asboe D. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. Jama. 2016 Jul 12;316(2):171-81.
6 Jin F, Prestage GP, Imrie J, Kippax SC, Donovan B, Templeton DJ, Cunningham A, Mindel A, Cunningham PH, Kaldor JM, Grulich AE. Anal sexually transmitted infections and risk of HIV infection in homosexual men. Journal of Acquired Immune Deficiency Syndromes. 2010;53:144-9.
7 Bavinton BR, Pinto AN, Phanuphak N, Grinsztejn B, Prestage GP, Zablotska-Manos IB, Jin F, Fairley CK, Moore R, Roth N, Bloch M. Viral suppression and HIV transmission in serodiscordant male couples: an international, prospective, observational, cohort study. The Lancet HIV. 2018 Aug 1;5(8):e438-47.
8 Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, Degen O, Corbelli GM, Estrada V, Geretti AM, Beloukas A, Raben D. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. The Lancet. 2019 Jun 15;393(10189):2428-38.
9 Callander D, McManus H, Gray RT, Grulich AE, Carr A, Hoy J, Donovan B, Fairley CK, Holt M, Templeton DJ, Liaw ST, McMahon JH, Asselin J, Petoumenos K, Hellard M, Pedrana A, Elliott J, Keen P, Costello J, Keane R, Kaldor J, Stoové M, Guy R. HIV treatment-as-prevention and its effect on incidence of HIV among cisgender gay, bisexual, and other men who have sex with men in Australia: a 10-year longitudinal cohort study. Lancet HIV. 2023 Jun; PMID: 37068498.
10 Gray RT, Wilson DP, Guy RJ, Stoové M, Hellard ME, Prestage GP, et al. Undiagnosed HIV infections among gay and bisexual men increasingly contribute to new infections in Australia. J Int AIDS Soc. 2018;21(4):e25104.
11 Jamil MS, Prestage G, Fairley CK, Grulich AE, Smith KS, Chen M, Holt M, McNulty AM, Bavinton BR, Conway DP, Wand H. Effect of availability of HIV self-testing on HIV testing frequency in gay and bisexual men at high risk of infection (FORTH): a waiting-list randomised controlled trial. The lancet HIV. 2017 Jun 1;4(6):e241-50.
12 Holt M, Lea T, Asselin J, Hellard M, Prestage G, Wilson D, et al. The prevalence and correlates of undiagnosed HIV among Australian gay and bisexual men: results of a national, community-based, bio-behavioural survey. J Int AIDS Soc. 2015;18(1):20526.
13 Grulich AE, Guy R, Amin J, Jin F, Selvey C, Holden J, Schmidt HMA, Zablotska I, Price K, Whittaker B, Chant K, Cooper C, McGill S, Telfer B, Yeung B, Levitt G, Ogilvie E, Dharan NJ, Hammoud MA, Vaccher S, Watchirs-Smith L, McNulty A, Smith DJ, Allen DM, Baker D, Bloch M, Bopage RI, Brown K, Carr A, Carmody CJ, Collins KL, Finlayson R, Foster R, Jackson EY, Lewis DA, Lusk J, O’Connor CC, Ryder N, Vlahakis E, Read P, Cooper DA, for the Expanded PrEP Implementation in Communities New South Wales (EPIC-NSW) research group. Population-level effectiveness of rapid, targeted, high-coverage roll-out of HIV pre-exposure prophylaxis in men who have sex with men: the EPIC-NSW study. Lancet HIV, 2018;5:e629-37
14 Grulich AE, Jin F, Bavinton BR, Yeung B, Hammoud MA, Amin J, Cabrera G, Clackett S, Ogilvie E, Vaccher S, Vickers T, McNulty A, Smith DJ, Dharan NJ, Selvey C, Power C, Price K, Zablotska I, Baker DA, Bloch M, Brown K, Carmody CJ, Carr A, Chanisheff D, Doong N , Finlayson R, Lewis DA, Lusk J, Martin S, Ooi C, Read P, Ryder N, Smith D, Tuck Meng Soo C, Templeton DJ, Vlahakis E, Guy R, for the Expanded PrEP Implementation in Communities New South Wales (EPIC-NSW) research group. Long-term protection from HIV infection with oral HIV pre-exposure prophylaxis in gay and bisexual men: findings from the expanded and extended EPIC-NSW prospective implementation study. Lancet HIV 2021; 8, e486-e494. PMID 34217426
15 Prevention Access Campaign. Risk of sexual transmission of HIV from a person living with HIV who has an undetectable viral load messaging primer & consensus statement. 2016. Accessed 21 March, 2025. https://preventionaccess.org/wp-content/uploads/2021/07/UU-Consensus-Statement.pdf
16 World Health Organization. Guidelines on HIV self-testing and partner notification: supplement to consolidated guidelines on HIV testing services. InGuidelines on HIV self-testing and partner notification: supplement to consolidated guidelines on HIV testing services 2016.
17 HIV self-tests available in Australia | Therapeutic Goods Administration (TGA)
18 PBS (Pharmaceutical Benefits Scheme). December 2017 PBAC (Pharmaceutical Benefits Advisory Committee) Meeting – Positive Recommendations. 2017. Accessed 9 December, 2024. https://www.pbs.gov.au/industry/listing/elements/pbac-meetings/pbac-outcomes
19 ASHM (Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine). National PrEP Guidelines Update: Prevent HIV by Prescribing PrEP. 2023. Accessed 9 December, 2024. https://prepguidelines.com.au
20 Chan C; Vaccher S; Fraser D; Grulich AE; Holt M; Zablotska-Manos I; Prestage GP; Bavinton BR, 2022, 'Preferences for Current and Future PrEP Modalities Among PrEP-Experienced Gay and Bisexual Men in Australia', AIDS and Behavior, 26, pp. 88 - 95, http://dx.doi.org/10.1007/s10461-021-03344-3
21 Holt, M., Chan, C., Broady, T. R., MacGibbon, J., Mao, L., Smith, A., Rule, J., & Bavinton, B. R. (2024). Variations in HIV prevention coverage in subpopulations of Australian gay and bisexual men, 2017-21: implications for reducing inequities in the combination prevention era. AIDS and Behavior, 28, 1469-1484.
22 Holt M, Broady TR, Mao L, Chan C, Rule J, Ellard J, O’Donnell D, Grulich AE, Prestage G, Bavinton BR. Increasing preexposure prophylaxis use and ‘net prevention coverage’ in behavioural surveillance of Australian gay and bisexual men. AIDS. 2021 Apr 1;35(5):835-40.
23 Gray, Richard T., Jo Watson, Aaron J. Cogle, Don E. Smith, Jennifer F. Hoy, Lisa A. Bastian, Robert Finlayson, et al. “Funding Antiretroviral Treatment for HIV-Positive Temporary Residents in Australia Prevents Transmission and Is Inexpensive.” Sexual Health 15, no. 1 (2017): 13–19. https://doi.org/10.1071/SH16237
24 Schneider, Karen, Richard T Gray, and David P Wilson. “A Cost-Effectiveness Analysis of HIV Pre-Exposure Prophylaxis for Men Who Have Sex with Men in Australia.” Clinical Infectious Diseases 58 (April 2014): 1027–34
25 Kerr, Cliff C, Robyn M Stuart, Richard T Gray, Andrew J Shattock, Nicole Fraser-Hurt, Clemens Benedikt, Markus Haacker, et al. “Optima: A Model for HIV Epidemic Analysis, Program Prioritization, and Resource Optimization.” JAIDS Journal of Acquired Immune Deficiency Syndromes 69, no. 3 (2015): 365–76.
26 Gray RT. Impact of increased antiretroviral therapy use during the treatment as prevention era in Australia. Sex Health. 2023;20(3):202–10. doi:10.1071/SH23088.
27 Petoumenos K, Watson J, Whittaker B, Hoy J, Smith D, Bastian L, Finlayson R, Sloane A, Wright ST, McManus H, Law MG. Subsidized optimal ART for HIV‐positive temporary residents of Australia improves virological outcomes: results from the Australian HIV Observational Database Temporary Residents Access Study. Journal of the International AIDS Society. 2015 Jan;18(1):19392.
28 Gray RT, Watson J, Cogle AJ, Smith DE, Hoy JF, Bastian LA, Finlayson R, Drummond FM, Whittaker B, Law MG, Petoumenos K. Funding antiretroviral treatment for HIV-positive temporary residents in Australia prevents transmission and is inexpensive. Sexual health. 2017 Sep 6;15(1):13-9.
29 Australian Government Department of Health and Aged Care. Ninth National HIV Strategy 2024–2030. Canberra: Department of Health and Aged Care; 2024
30 Bavinton BR, Jin F, Mao L, Zablotska I, Prestage GP, Grulich AE. Homosexual men in HIV serodiscordant relationships: implications for HIV treatment as prevention research. African Journal of Reproduction and Gynaecological Endoscopy. 2015 Jan 1;18(1)
31 Bavinton BR, Holt M, Grulich AE, Brown G, Zablotska IB, Prestage GP. Willingness to act upon beliefs about ‘treatment as prevention’ among Australian gay and bisexual men. PloS one. 2016 Jan 7;11(1):e0145847
32 Philpot SP, Prestage G, Ellard J, Grulich AE, Bavinton BR. How do gay serodiscordant couples in Sydney, Australia negotiate undetectable viral load for HIV prevention?. AIDS and Behavior. 2018 Dec;22:3981-90
33 Prestage G, Maher L, Grulich A, Bourne A, Hammoud M, Vaccher S, Bavinton B, Holt M, Jin F. Brief report: changes in behavior after PrEP initiation among Australian gay and bisexual men. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2019 May 1;81(1):52-6
34 MacGibbon J, Broady T, Drysdale K, Bavinton B, Lee E, Mao L, Prestage G, Holt M. Gay men’s relationship agreements in the era of pre-exposure prophylaxis: An analysis of Australian behavioural surveillance data. AIDS and Behavior. 2020 May;24:1389-99
35 Bavinton BR, Grulich AE, Broady T, Keen P, Mao L, Patel P, Chan C, Prestage GP, Holt M. Increases in HIV testing frequency in Australian gay and bisexual men are concentrated among PrEP users: An analysis of Australian behavioural surveillance data, 2013–2018. AIDS and Behavior. 2020 Sep;24:2691-702
36 Bavinton BR, Hammoud MA, Holt M, Saxton P, Bourne A, MacGibbon J, Jin F, Maher L, Prestage GP. Changes in sexual behaviour following PrEP initiation among Australian gay and bisexual men in relationships: results from a prospective observational study. AIDS and Behavior. 2021 Nov 1:1-8
37 MacGibbon J, Bavinton BR, Broady TR, Ellard J, Murphy D, Calabrese SK, et al. Familiarity with, perceived accuracy of, and willingness to rely on Undetectable=Untransmittable (U=U) among gay and bisexual men in Australia: results of a national cross-sectional survey. Sex Health. 2023;20(3):211-22.
38 King J, McManus H, Kwon A, Gray R, McGregor S. HIV, viral hepatitis and sexually transmissible infections in Australia: annual surveillance report 2022. Sydney: The Kirby Institute, UNSW Sydney. 2022.
39 Holt M, Broady TR, Mao L, Chan C, Rule J, Ellard J, et al. Increasing preexposure prophylaxis use and ‘net prevention coverage’ in behavioural surveillance of Australian gay and bisexual men. AIDS. 2021;35(5):835-40.
41 HIV self-testing strategic framework: a guide for planning, introducing and scaling up. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO
42 AVAC. HIV Rapid Diagnostic Test Market Landscape, 2023. New York: PrEPWatch; 2024 Sep 23 [cited 2025 Jul 4]. Available from: https://www.prepwatch.org/wp-content/uploads/2024/09/EIC-HIV-Market-Landscape-Report.pdf