Focus Areas are the thematic domains for the Actions that will deliver on the Goals of the National Strategy.
Table of contents
This is a draft of the National Health and Medical Research Strategy.
Focus areas – actions to drive transformational change
Build a vibrant research system that delivers for the nation
National priority setting and evaluation: Embed consistent processes to set, fund and evaluate research impact against national priorities, overseen and supported by a National Strategy Advisory Council.
Horizon scanning: Establish mechanisms for identifying new and emerging challenges for the health system that inform and guide priority setting, investment and workforce and infrastructure planning.
Collaborative platforms and networks: Prioritise collaborations and sharing of resources, through investment in platforms and networks across the health and medical research ecosystem, to support research, workforce development and translation in areas of national priority.
Embed research processes that are modern, efficient and consumer centred
Commonwealth research funding: Establish unified management of the Medical Research Endowment Account (MREA) and Medical Research Future Fund (MRFF) to ensure strategic, coordinated investment, aligned to national health priorities and challenges.
Clinical trials: Enable a vibrant clinical trials sector that improves patient outcomes and supports equitable access to clinical trials, regardless of demography or geography.
Consumer and community involvement: Reward inclusivity and embrace diversity – particularly for priority populations – and build community trust in health and medical research.
Regional, Rural, and Remote (RRR) research: Develop research processes that are adaptable and flexible to respond to the unique needs, challenges and opportunities of RRR communities
Accelerate research and its translation to improve Aboriginal and Torres Strait Islander Peoples’ health and wellbeing
Aboriginal and Torres Strait Islander Peoples’ ways of knowing, being and doing: Build community-led, place-based, co-designed research and translation activities, supported by consolidated and coordinated funding opportunities.
Translation and implementation: Prioritise community-based, innovative solutions to implement research outcomes that address the National Agreement on Closing the Gap.
Aboriginal and Torres Strait Islander leadership and workforce capacity and capability building: Enhance Aboriginal and Torres Strait Islander health and medical research leadership and support emerging researchers, particularly community-based researchers with non-traditional pathways into research.
Drive impact through research translation, innovation and commercial solutions
Research translation: Develop and expand on current structural solutions and initiatives, such as Research Translation Centres and hub and spoke models, to embed translation and research expertise in healthcare settings.
Industry integration and risk sharing: Establish mechanisms that optimise research-industry exchange and moderate and share risk for industry to stimulate investment attractiveness and drive commercial outcomes.
Manufacturing and marketing: Support commercialisation and sovereign capability by building local biotech and medtech manufacturing and industry marketing capabilities and research-industry partnerships for national and international markets.
Position to be ready for future needs and challenges
Emerging technology: Build capability and capacity to take advantage of innovative emerging technologies including cutting edge approaches for responsible and impactful harnessing of AI.
Environmental sustainability: Consider the impact of health and medical research and health system outcomes on climate as a key factor in priority setting and embed research processes that promote environmental sustainability
Global partnerships: Promote strategic collaborations that address shared health priorities and strengthen Australia’s leadership globally and in the Indo-Pacific region.
Focus area 1: Build a vibrant research system that delivers for the nation
Overview
Coordination of priorities and investment strategies across all health and medical research funders, with a focus on horizon scanning, partnerships and shared infrastructure will build a vibrant health and medical research system. This system will deliver impactful research that improves the health of Australians and contributes to national productivity and sustainability, now and in the future.
| Drive national prosperity and security | A vibrant research system that incorporates priority setting and evaluation activities, platforms and networks and horizon scanning will drive national prosperity and security. |
|---|---|
| Lead the world in health outcomes | A research ecosystem that delivers for the nation with a focus on coordination of priority setting, investment activities and partnerships will place Australia as a global leader in world health outcomes. |
| Deliver equity – no one left behind | Priority setting which is inclusive of all populations, irrespective of socioeconomic status or geographic location will ensure equitable health outcomes are achieved. |
| Secure a resilient and a sustainable health system | The resilience and sustainability of Australia’s health system will be strengthened through a national approach to priority setting and a focus on translation |
| Strengthen regional and global partnerships | Regional and global partnerships are a key foundation of a research system that delivers for the nation, building access to new technologies and practices that improve outcomes. |
National priority setting and evaluation
Research funding decisions – whether made by the Commonwealth, states and territories, industry, or philanthropic organisations – should be driven by priorities that offer the greatest potential benefit to public health and community wellbeing. When these priorities are nationally aligned, there are opportunities to generate efficient research outcomes. A coordinated process of priority setting and evaluation, guided by evidence and community needs, can ensure that limited resources are used efficiently and fairly. It is also important to regularly assess whether funded research is delivering results as expected and whether the systems in place are effectively supporting the translation of research into real world outcomes.12
Horizon scanning
Horizon scanning is a critical tool in cultivating a vibrant research system, especially in the face of rapidly emerging challenges and transformative technologies. By systematically exploring potential future developments, horizon scanning can guide researchers, policymakers and institutions to anticipate shifts in scientific, technological, and societal landscapes over the next decade.13 Ultimately, horizon scanning supports decision making processes14, strengthens the foundation of a forward looking research ecosystem that is equipped to address complex problems and harness new technologies that will deliver benefits for all.
Collaborative platforms and networks
Platforms and networks provide the infrastructure and connectivity required to bring together scientists, researchers, clinicians, policymakers and communities across the health and medical research ecosystem. By facilitating data sharing, resource pooling and coordinated research efforts on a larger scale and for longer time periods, platforms and networks accelerate innovation, reduce duplication and enhance the translation of research outcomes.
A fundamental aim of the Australian health system is to prevent disease, intervene early and reduce ill health, enabling people to live in good health, for as long as possible. Population groups that experience social inequalities and disadvantage resulting in health inequality are considered priority populations. These include Aboriginal and Torres Strait Islander peoples, Culturally and Linguistically Diverse (CALD) people, LGBTIQ+ people, people with a disability, people with mental health conditions, people in low socioeconomic groups and people living in regional, rural or remote areas.15 A vibrant research system needs to account for these population groups at all stages of the research process including priority setting and evaluation, horizon scanning and investments in platforms and networks.
National priority setting and evaluation
Embed consistent processes to set, fund and evaluate research impact against national priorities, overseen and supported by a National Strategy Advisory Council.
How we could do it
- Foster coordinated, formalised communication and collaboration across Commonwealth and state and territory governments to align priority setting in a way that will develop streamlined, scalable, co-investment strategies supportive of shared outcomes and long-term impact.
- Implement mechanisms to ensure industry, philanthropy, researchers, consumers and communities are engaged in the ethical priority setting of health and medical research.
- Ensure balanced investment into investigator-led and priority-driven research, across discovery, clinical, translational and commercialisation research and development, with fair funding practices that reinforce a positive culture of inquiry and learning.
- Embed research priority frameworks that are aligned with long-term, health system-wide goals. These frameworks will incorporate the needs of priority populations and those under-represented in the current system (for example, research into rare diseases) and be robustly guided by ethical principles.16
- Establish nationally aligned impact measurement tools – including adopting comprehensive models in addition to traditional academic metrics – to evaluate real world outcomes, health system improvements, economic returns, and societal benefits of research.
- Establish a National Strategy Advisory Council to uphold the values, oversee the implementation and measure the success of the National Strategy.
Why we should do it
- A nationally coordinated health and medical research system will be more streamlined and resource efficient to maximise impact through collaboration across governments, industry, academic, health care, philanthropic and community sectors.
What it could achieve
- Priorities that are inclusive, equitable and aligned to community needs.
- Research funding that is strategically directed towards identified areas of need.
- Investment practices that achieve the right distribution of funds across discovery and priority-driven research.
- Unified and impact-driven funding landscape for Australian health and medical research through increased collaboration across funders.
- A responsive and needs based research funding system that can adapt to the changing global health environment.
- Increased impact and accountability of Australian health and medical research.
NSW Setting Research Priorities17
The NSW government has produced a guide to assist NSW Health staff to identify and update population health research priorities. The guide includes information regarding: the purpose of setting research priorities; principles of effective research priority setting; and a suggested process for setting, disseminating and reviewing research priorities. The guide provides users with a 4 stage process for setting and reviewing research priorities including:
- Background investigation and preparation;
- Generate and refine research priorities;
- Finalise and disseminate research priorities;
- Review and update research priorities.
James Lind Alliance (JLA)18
JLA is a UK based nonprofit initiative that was established in 2004. The JLA process is focused on bringing patients, carers and clinicians together, on an equal basis, in a priority setting partnership (PSP) to define and prioritise uncertainties relating to a specific condition or health setting. It aims to raise awareness among research funding groups about what matters most to patients, carers and clinicians, to ensure that clinical research is both relevant and beneficial to end users.
Horizon scanning
Establish mechanisms to identify new and emerging challenges for the health system that inform and guide priority setting, investment and workforce and infrastructure planning.
How we could do it
- Establish a nationally coordinated horizon scanning mechanism across Commonwealth, state and territory jurisdictions to identify emerging health challenges, research opportunities and areas of unmet need, and to assist in priority setting, investment and workforce and infrastructure planning. This work would occur in collaboration with the Australian Centre for Disease Control in safeguarding Australia from health threats.
- Establish robust policy frameworks that integrate emerging risks and challenges identified through the coordinated horizon scanning mechanism, to inform policy and program development across the Enablers of Workforce, Funding, Data and Infrastructure.
Why we should do it
- Australia’s health system faces a range of challenges including an ageing population and the associated increasing demand on health services, increasing rates of chronic disease and rising costs of medical research and innovations.
- Key global health threats must be anticipated, including outbreaks of vaccine-preventable diseases, increasing reports of drug-resistant pathogens and the health impacts of environmental pollution and climate change.
- We must also take advantage of available data, emerging technologies and modernised practices.
- When performed consistently and effectively, horizon scanning, in partnership with other forecasting tools, can assist policy making and program design.
What it could achieve
- A unified and strategic approach to identifying and responding to emerging challenges, research opportunities and areas of unmet need.
- The ability for governments, industry, philanthropic and research organisations to make informed strategic decisions across the health and medical research ecosystem.
Horizon scanning and landscape analysis by the World Health Organization (WHO)19
The WHO recommends horizon scanning or landscape analysis for a range of purposes, such as preparation for research prioritisation and driving research directions by indicating gaps and forming the basis for research agenda setting. A key WHO landscape analysis is the annual antimicrobial resistance R&D landscape analysis, which evaluates the pipeline of antibacterial candidates in development.
Australian Centre for Disease Control (ACDC)20
CDC’s horizon scanning for new and emerging human health threats takes a One Health approach, where policies and programs recognise the intrinsic link between the health of humans, animals and the environment. Horizon scanning activities are undertaken collaboratively with ACDC’s key One Health partners including other Australian Government departments, state and territory governments, First Nations organisations, Wildlife Health Australia and the Commonwealth Scientific and Industrial Research Organisation (CSIRO).
Collaborative platforms and networks
Prioritise collaborations and sharing of resources, through investment in platforms and networks across the health and medical research ecosystem, to support research, workforce development and translation in areas of national priority.
How we could do it
- Prioritise longer term health and medical research funding through a platform and network based approach. Creating incentives to develop collaborative infrastructure, multidisciplinary partnerships and efficient resource utilisation can deliver major impact across the health and medical research ecosystem.
- Establish processes to identify and fund new networks and platforms that align to national priority areas and community need. Embedding assessment criteria and governance mechanisms within national policy frameworks to evaluate the relevance, scalability and collaborative potential of specific research initiatives will assist in these processes.
Why we should do it
- Research networks bring together health and medical professionals, scientists, researchers, service providers and consumers and community members to drive impact through place-based and virtual collaborations.
- Networks can improve the opportunities for research participation and increase equity of outcomes.
- Centralised platforms often provide shared infrastructure, tools, or services that can be accessed by multiple projects or users, reducing the need to build systems from scratch and allowing for more broadly consistent standards and practices.
- Technology networks and platforms often support integration with other systems, allowing data and tools to work together seamlessly. Research supported through linked data within these networks can lead to improved health outcomes.
What it could achieve
- Strategic and targeted investment through platforms and networks to address areas of national priority, where collaborative models are most likely to deliver long term results
- A strong Australian health and medical research ecosystem where collaborative, equitable, platform-based models aligned to need increase the effectiveness of research and create pathways to scaled implementation.
The NSW-funded RNA Production and Research Network21
This Network enables access for scientists to materials required to translate newly developed RNA therapeutics from the bench to advanced pre-clinical studies. It supports production linked to therapeutic research and is building capacity and capability as a prerequisite to downstream Good Manufacturing Practice.
Bioplatforms Australia22
Supports biomedical and human health research in Australia by leveraging the cutting-edge integrated technologies operated across the national laboratory and bioinformatics network. These technologies enable the generation of large scale (usually population level) data resources and secure data sharing solutions required to advance the understanding and treatment of complex diseases and conditions spanning cancers, cardiovascular diseases, antimicrobial resistance as well as health related functions associated with gut metabolites and microbiomes.
Examples of national collaborative projects supported through Bioplatforms Australia include: Australian Psychiatric Research Knowledge Bank; Ricin genomics and global origins initiative; Australian Function Fungi Initiative; Australian Gut Metabolome Initiative; Indigenous genomics; Cardiovascular Framework Initiative; Sepsis; Aspirin in reducing events in the elderly (ASPREE) Framework Initiative; Exceptional responders; Melanoma; and Stem cells.22
Focus area 2: Embed research processes that are modern, efficient and consumer centred
- Commonwealth research funding
- Clinical trials
- Consumer and community involvement
- Regional, rural and remote research
Overview
Well-coordinated, modern, efficient research processes that reduce administrative burden on researchers and drive consumer engagement and co-design will enable a more effective and sustainable health and medical research sector.
| Drive national prosperity and security | Unified, aligned and coordinated management of MRFF and MREA funding provides an avenue for public funds to be used efficiently to effectively deliver maximum impact |
|---|---|
| Lead the world in health outcomes | A successful Australian environment for clinical trials will identify innovative treatments and technologies, contributing to improved care and better health outcomes. |
| Deliver equity – no one left behind | Meaningful consumer and community involvement will support research that meets the needs of the community and ensures that trust, diversity, geographic reach and equity are central. |
| Secure a resilient and a sustainable health system | Aligning the MREA and MRFF, including processes to drive consumer and community involvement and strengthening clinical trials, will position Australia to respond swiftly to emerging challenges. |
| Strengthen regional and global partnerships | A well-coordinated Australian approach to health and medical research will set the foundation to build and strengthen regional and global partnerships |
Efficient management of Commonwealth research funding
Efficient and unified management of the two primary Commonwealth health and medical research funds (MREA and MRFF) will ensure investment aligns with national health priorities and emerging challenges. Harmonising funding cycles, reporting processes and impact expectations across Commonwealth schemes will reduce duplication, avoid funding gaps and streamline application processes, ultimately lowering administrative burden and improving transparency. This will provide opportunities for non-Commonwealth funders to align funding processes and procedures, leading to broader efficiency.
Enabling a vibrant clinical trials sector
A flourishing clinical trials sector and further embedding research into routine care will advance Australia’s health and medical research outcomes and increase equitable access to innovative therapeutics and interventions. A strong clinical trials ecosystem that is underpinned by the NOSS, and growth of Clinical Trial Networks, can reduce costs through efficient trial design and accelerate the translation of evidence into practice. Developing sovereign capacity in clinical trial management can bring innovation into practice more quickly.
Driving consumer and community involvement in research
The National Health and Medical Research Community Qualitative Research report23 found that many Australians believe the general public should have a say in research priority areas. A range of involvement options should be provided to overcome barriers such as time constraints and the expectation to understand overly complex information. Opportunities and communications must be tailored to the needs and interests of certain communities; for example, activities to involve Aboriginal and Torres Strait Islander peoples should implement culturally safe practices and take a localised approach in their design.
Responding to the needs of RRR research
Nearly 7 million Australians live in regional, rural and remote areas and, on average, experience poorer health outcomes and shorter life expectancy due to limited access to healthcare and the effects of the social determinants of health.24 To improve equity, research in these communities must overcome barriers like distance, workforce shortages and infrastructure gaps, with adaptable approaches that build lasting, locally embedded research capacity.
An important area of feedback from the research sector during consultation on the National Strategy has been the need for greater support to meet the full costs of conducting research. These costs can include equipment, infrastructure and bridging salary gaps for researchers. We have heard that the increasingly sophisticated and complex nature of research is leading to indirect costs that are outstripping block funding and other support mechanisms. Reducing the impact of indirect costs will require a whole of sector approach, supported by the National Strategy. Opportunities include approaches that direct funding towards indirect costs that are currently not supported by existing mechanisms, infrastructure sharing or new cost effective platform and network approaches for highly specialised equipment. Better understanding the flow of funding and existing funding gaps, as well as encouraging collaborative research to minimise duplication, will also support sustainability and reduce the burden of indirect costs for the sector.
Commonwealth research funding
Establish unified management of the MREA and MRFF to ensure strategic, coordinated investment, aligned to national health priorities and challenges.
How we could do it
- Bring together management of the MREA and the MRFF under a single executive agency.
- Ensure that the unique strengths of each fund are preserved, while delivering administrative efficiency, addressing duplication and gaps and driving research excellence from discovery science to translation.
- Stronger coordination and alignment with other organisations and processes, such as the Australian Research Council (ARC) and output of the SERD, where possible, including:
- key policies, such as those related to consumer and community involvement and open access to funded research outputs
- research processes, including funding cycles, application and assessment processes, reporting, evaluation and impact measurement.
Why we should do it
- Consultation on the National Strategy has supported findings from a recent review of the major Commonwealth health and medical research funding mechanisms which sought to improve alignment and coordination between the MREA and the MRFF25, in particular:
- A prevailing view that the 2 funds should be managed by a single executive agency.
- The need for a ‘seamless but not homogenous’ funding model – where the best of both funds is preserved and brought together in closer alignment and coordination.
- The desire for a transparent, strategic, cohesive and fit for purpose funding system, including balanced support across the entire research pipeline and new avenues for consumer and community engagement.
What it could achieve
- Coordinated, transparent, and fit for purpose investment through one unified Commonwealth health and medical research executive agency.
- A consistent set of research processes, reducing administrative burden on the sector.
- Synergies and efficiencies through streamlined administrative management, leading to better visibility of the funding landscape to enable the development of a resourcing statement (see Funding Enabler).
- Consistent policies and mechanisms to embed diversity and equity in research.
- An opportunity to improve understanding in the community through a ‘front door’ of Australian Government funded health and medical research.
NHMRC/MRFF joint advisory committees26
Following the consultation on MRFF-MREA alignment, 4 joint committees were established to advise on research strategies and policies for both funds, harmonising and improving coordination, integrating skills sets and experiences to optimise advice about different kinds of research:
- Consumer Advisory Group – advises on consumer and community involvement in health and medical research (HMR), including on strengthening consumer involvement in MREA and MRFF grant programs.
- Industry, Philanthropy and Commercialisation Committee – advises on industry and philanthropic involvement in HMR and strategies to foster greater research commercialisation.
- Public Health and Health Systems Committee – advises on strategies for strengthening preventive health, public health, primary care and health services, and for embedding research translation in the Australian health system.
- Indigenous Advisory Group – advises on Aboriginal and Torres Strait Islander health research and capacity building for Indigenous health researchers.
Unified administration of health and medical research27
UK Research and Innovation (UKRI) is an overarching public body that directs research and innovation (R&I) funding in the UK. It was created in 2018 with the aim of increasing integrative cross-disciplinary research. UKRI brings together 7 disciplinary research councils (including the Medical Research Council), Innovate UK and Research England into one unified body. This enables UKRI to work across the whole R&I system, and to connect research communities, institutions, businesses and wider society, in the UK and around the world.
This approach to unified administration has proven successful for various research efforts. An impact evaluation of the UKRI’s COVID-19 response found that the nature of the UK R&I landscape played a substantial role in enabling a robust and timely response across multiple research areas and the realisation of wide ranging social and economic impacts.
Clinical trials
Enable a vibrant clinical trials sector that improves patient outcomes and supports equitable access to clinical trials regardless of demography or geography.
How we could do it
- System and regulatory reform, and growth in Clinical Trials Networks, to support equitable access to clinical trials, encourage innovation, develop sovereign capability and improve the quality of healthcare in Australia.
- Implementation of the National One Stop Shop for Clinical Trials and the National Clinical Trials Governance Framework across public and private health services.
- Roll out the Human Research Ethics Committee Quality Standard and Accreditation Scheme.
- Invest in regional, rural and remote clinical trial infrastructure, including long term funding for Clinical Trial Networks to manage logistics, data and recruitment.
Why we should do it
- Clinical trials are a core part of a learning health system and evidence-based medicine – they are essential for the development of, and access to, new treatments and innovations. Australia is an attractive place to undertake trials and compares favourably to other OECD countries in terms of clinical trial activity, which has been increasing, with new studies registered per year rising from 725 in 2006 to 1,349 in 2020.28
- To help reduce health disparities and better inform clinical and public health decision making, participation in clinical trials needs to be inclusive and representative.
- Between 2006 and 2021, 0.8% of registered trials had an exclusive focus on the health of Aboriginal and Torres Strait Islander peoples and communities, but there is little available detail on the inclusion of Aboriginal and Torres Strait islander people in trials more generally.28
- Despite culturally and linguistically diverse Australians representing almost a third of the population, research has shown they are often excluded from clinical research due to potential lack of fluency in English being considered a risk to informed consent.29
- Until the 1990s, women were routinely excluded from clinical trials due to assumptions about reproductive risks and the impact of hormonal differences on trial findings. As a result, the underrepresentation of sex and gender differences in research data remains an issue.30-32
- There are opportunities to improve access to trials in Australia through regulatory system reforms and growth in clinical trial networks.
- The economic benefits of clinical trials are notable; an economic evaluation of 25 investigator-initiated clinical trials conducted across 3 clinical trial networks found that:33
- There was a return of $5.80 for every $1 invested in the networks.
- If results from these trials were implemented in 65% of the eligible Australian patient populations for one year, this would deliver a net benefit of $1.6 billion (2014 dollars).
What it could achieve
- Better inclusion and diversity in trials, including through incentives and broader representation, especially for rural, Aboriginal and Torres Strait Islander, and other underserved communities.
- Stronger integration between research and healthcare delivery, including through increased clinician engagement in clinical trial activities.
- Development and growth of regional health infrastructure, including trial sites, telehealth capabilities and mobile research units.
- Faster access to cutting edge therapies for patients across Australia.
- Central, coordinated expertise to equip researchers and clinicians with the capability and capacity to get trials up and running.
Breast Cancer Trials34
 Breast Cancer Trials (BCT) is the largest independent oncology clinical trials research organisation in Australia and New Zealand, dedicated to the prevention, treatment and cure of breast cancer. Founded in 1978, BCT conducts a multi-centre national and international clinical trials research program involving over 1,014 researchers across 118 institutions in Australia and New Zealand. This unique collaboration between researchers, clinical trial participants and supporters has involved more than 17,910 participants in 95 clinical trials and led to improvements in the treatment and management of breast cancer and lives saved.
Breast Cancer Trials (BCT) is the largest independent oncology clinical trials research organisation in Australia and New Zealand, dedicated to the prevention, treatment and cure of breast cancer. Founded in 1978, BCT conducts a multi-centre national and international clinical trials research program involving over 1,014 researchers across 118 institutions in Australia and New Zealand. This unique collaboration between researchers, clinical trial participants and supporters has involved more than 17,910 participants in 95 clinical trials and led to improvements in the treatment and management of breast cancer and lives saved.
Consumer and community involvement
Reward inclusivity and embrace diversity – particularly for priority populations – and build community trust in health and medical research.
How we could do it
- Coordinate nationally to prioritise inclusion of diverse and priority populations, by co-designing research agendas, using inclusive recruitment strategies, increased support and capacity building for the sector and providing fair compensation.
- Build infrastructure/mechanisms for greater Consumer and Community Involvement (CCI), such as CCI networks and digital platforms.
- Monitor, evaluate and disseminate information about research impact to the broader community.
- Uphold and support implementation of the NHMRC Statement on CCI in health and medical research and the principles for consumer involvement, in all health and medical research.
Why we should do it
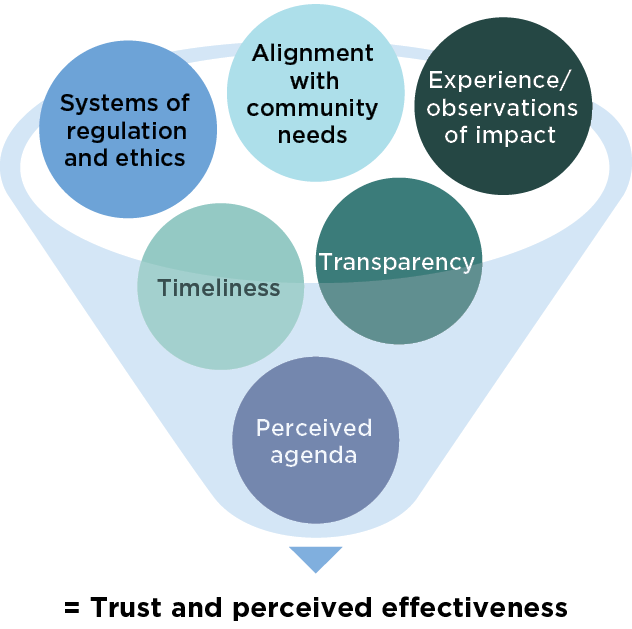
Meaningful involvement of community and consumers across all stages of health and medical research, from priority setting to translation, enhances the relevance, quality and impact of research outcomes, particularly for priority populations. Partnering with consumers and communities provides an opportunity to build trust in science and social licence for research.
What it could achieve
- Research that is shaped by, and benefits, the communities it affects.
- Consistent frameworks and training across institutions for inclusive research practices.
- Increased involvement of priority and underserved populations.
- Improved public trust and social licence in health and medical research.
- Research that addresses the social determinants of health and systemic barriers to reduce health disparities.
- Institutional and cultural transformation, including through recognition and reward systems for researchers who demonstrate excellence in community engagement.
WA Consumer and Community Involvement Program (CCIProgram)35
![]()
The CCIProgram, based out of the WA Health Translation Network, supports consumers, community members and researchers to work in partnership to make decisions about health research, policy and practice. The CCIProgram also provides tailored CCI support for research, unique involvement opportunities, and a diverse range of capacity building activities and engagement events. In 2023–24, there were over 6,000 members with lived experience interested in informing health and medical research. The CCIProgram supported the development of WA’s first Mental Health Research Framework, enabling people with lived experience of mental health challenges to play a pivotal role in establishing priorities for mental health research.
National Centre for Indigenous Genomics (NCIG)36
 NCIG was formed at the recommendation of leading Indigenous Australian thinkers and advocates. The Australian National University put the future of a research collection in the hands of an Indigenous consultative committee, agreeing to abide by their recommendations. The consultative committee regarded the collection as having immense cultural, historical and scientific importance. The NCIG’s genome research is conducted in line with customary laws and practices and community interests. Indigenous Australians play the central role in decisions about data collection, stewardship, access and use. They ensure that the conduct of research and dissemination of findings become part of cultural narratives that have meaning in the lives of Indigenous Australians.
NCIG was formed at the recommendation of leading Indigenous Australian thinkers and advocates. The Australian National University put the future of a research collection in the hands of an Indigenous consultative committee, agreeing to abide by their recommendations. The consultative committee regarded the collection as having immense cultural, historical and scientific importance. The NCIG’s genome research is conducted in line with customary laws and practices and community interests. Indigenous Australians play the central role in decisions about data collection, stewardship, access and use. They ensure that the conduct of research and dissemination of findings become part of cultural narratives that have meaning in the lives of Indigenous Australians.
'The enthusiasm with which communities are participating in NCIG research, when other research initiatives struggle to achieve effective participation, is powerful evidence that the NCIG approach is working.'
Regional, Rural and Remote (RRR) health and medical research
Develop research processes that are adaptable and flexible to respond to the unique needs, challenges and opportunities of RRR communities.
How we could do it
- Establish methods to ensure RRR research is consistently included in priority setting initiatives and ensure that priority setting engages effectively and meaningfully with local communities.
- Coordinate Commonwealth, state and territory agencies to establish affirmative action for research conducted in, with and by RRR researchers and communities.
- Develop local infrastructure and services to support clinician researchers in RRR areas to increase the translation of research in ways that are appropriate and fit for purpose for the communities and settings they service.
- Ensure that grant assessment processes have balanced representation from RRR researchers.
- Promote and incentivise research collaborations with RRR researchers, particularly to extend access to clinical trials and translational research activities in the community.
Why we should do it
Approximately 7 million Australians (approximately 27% of the population) live in RRR areas, and, on average, they experience worse health outcomes and shorter life expectancy than other Australians.24 There are multiple factors that contribute to health inequities for RRR populations, including poorer social determinants of health and reduced access to primary healthcare services.37
While engaging in research has demonstrated benefits for health outcomes, undertaking research in RRR areas faces significant barriers including distance, constrained clinical services, a limited research workforce and limited access to research infrastructure.38–42
Every RRR community in Australia is different and faces unique challenges in its degree of remoteness, health system capacity, demographics and healthcare needs. Therefore, research frameworks need to be adaptable and responsive to the specific needs of each community, with a focus on building and embedding enduring research capacity within the community and adopting smart approaches with new technological solutions to overcome vast distances.
What it could achieve
- Equitable research investment that helps to close long-standing gaps in health outcomes and research representation.
- Embedded local research capacity, ensuring that research expertise is grown and sustained within communities, rather than being externally driven or temporary.
- Community driven priorities for RRR research that reflect the real needs and values of local populations.
- Fit for purpose translation that works in real RRR settings.
- Fair representation in decision-making leading to more inclusive and context-aware funding decisions.
- Expanded access to innovation, including clinical trial access, will extend cutting edge research opportunities to RRR communities, improving health equity.
Townsville Institute of Health Research and Innovation (TIHRI)43
 The TIHRI is a purpose-built facility that supports all phases of clinical trials and strengthens local research capacity in northern Queensland. It provides infrastructure and resources for clinician researchers, including specialised equipment and collaborative spaces. TIHRI’s strategic plan emphasises digital health, First Nations inclusion and workforce development to address regional health challenges. As the only tertiary university hospital in the region, it exemplifies how locally embedded research can improve health outcomes in regional, rural, and remote communities.
The TIHRI is a purpose-built facility that supports all phases of clinical trials and strengthens local research capacity in northern Queensland. It provides infrastructure and resources for clinician researchers, including specialised equipment and collaborative spaces. TIHRI’s strategic plan emphasises digital health, First Nations inclusion and workforce development to address regional health challenges. As the only tertiary university hospital in the region, it exemplifies how locally embedded research can improve health outcomes in regional, rural, and remote communities.
Focus area 3: Accelerate research and its translation to improve Aboriginal and Torres Strait Islander Peoples’ health and wellbeing
- Aboriginal and Torres Strait Islander Peoples’ ways of knowing, being and doing
- Translation and implementation
- Aboriginal and Torres Strait Islander leadership and workforce capacity and capacity building
Overview
More community driven research led by Aboriginal and Torres Strait Islander health and medical researchers and removal of structural inequities to research translation will improve Aboriginal and Torres Strait Islander health outcomes.
| Drive national prosperity and security | Investment in Aboriginal and Torres Strait Islander health research is crucial to ensuring Australia's national prosperity and security by overcoming systemic social and health disparities so everyone can contribute to the economy. |
|---|---|
| Lead the world in health outcomes | Australia will only lead the world in health outcomes when there is health equity between Australian Aboriginal and Torres Strait Islander Peoples and non-Aboriginal Australians. |
| Deliver equity – no one left behind | Continued investment in community led research and translation that alleviates structural inequities will generate effective community-based solutions for everyone. |
| Secure a resilient and sustainable health system | Aboriginal and Torres Strait Islander knowledge should play a transformative role in building a sustainable health system by offering holistic, community centred and environmentally attuned approaches to health and wellbeing. |
| Strengthen regional and global partnerships | Prioritising Aboriginal and Torres Strait Islander leadership and knowledge in health and medical research means Australia can model how nations should engage Indigenous communities in global health governance. |
Aboriginal and Torres Strait Islander Peoples’ ways of knowing, being and doing
Research shows that having Aboriginal and Torres Strait Islander health in Aboriginal and Torres Strait Islander hands is the best model for positive health outcomes.44 This is why it is vital to invest more into research and translation activities that are community led and designed. Commonwealth investment in Aboriginal health research has been increasing through dedicated funding from the NHMRC and MRFF.45,46
Translation and implementation
The most recent report from the Productivity Commission on progress towards ‘Closing the Gap’ targets revealed that, while certain indicators were on track, such as proportion of babies born with a healthy birthweight, others, such as childhood development and improving social and emotional wellbeing, have worsened.47 More needs to be done to improve these indicators through innovative research and translation activities designed and led by Aboriginal and Torres Strait Islander communities.
Aboriginal and Torres Strait Islander leadership and workforce capacity and capability building
The sector has seen an increase in the number of Aboriginal and Torres Strait Islander chief investigators on research grants funded by the NHMRC and MRFF.45,48 More can be done to sustain the workforce by continued training and capability building of the next generation of experts. The achievements of the Lowitja Institute, Aboriginal community controlled health organisations (ACCHOs) and networks (e.g Our Collaborations in Health Research – OCHRe) require further support.
 Aboriginal and Torres Strait Islander health refers not just to the physical health of an individual but to the social, emotional and cultural wellbeing of the whole community.49
Aboriginal and Torres Strait Islander health refers not just to the physical health of an individual but to the social, emotional and cultural wellbeing of the whole community.49
The Mayi Kuwayu study50 is the largest national study of Aboriginal and Torres Strait Islander culture, health and wellbeing. Its development arose from Aboriginal and Torres Strait Islander Peoples’ and communities’ need to have robust evidence on the links between culture, health and wellbeing. Aboriginal and Torres Strait Islander cultural practice and expression, together with physical, emotional and community connections are recognised as a vital element to health and wellbeing. Over 13,000 Aboriginal and Torres Strait Islander peoples have responded by sharing their stories that recognise identity, spirituality, and connection to Country, community and language as fundamental elements of culture. The Study adheres to the Indigenous Data Sovereignty Principles.51 Outcomes to date include positive health associations with participating in a Ranger program; development and validation of culturally specific measures of discrimination, psychological distress, family functioning and cultural wellbeing; population-level contribution of discrimination to psychological distress; development of community data projects and development and delivery of data literacy training.
Aboriginal and Torres Strait Islander Peoples' ways of knowing, being and doing
Build community led, place based, co-designed research and translation activities, supported by consolidated and coordinated funding opportunities.
How we could do it
- Undertake ongoing reviews of the funding landscape for Aboriginal and Torres Strait Islander health research to ensure investments are meeting needs.
- This will be done in conjunction with the wider review of the health and medical research funding landscape (see Funding Enabling Initiative).
- Design consistent funding processes across funding organisations that include data needed to monitor trends (e.g. Aboriginal and/or Torres Strait Islander status of investigators).
- Create more pathways for community organisations to submit topics for grant opportunities such as NHMRC’s Targeted Calls for Research grant scheme.52
- Better coordinate and align policies related to funding for Aboriginal and Torres Strait Islander health research across government and with non-government funders. Ensure there is alignment with existing frameworks such as the NHMRC Road Map 3: A strategic framework for improving Aboriginal and Torres Strait Islander health through research.53
- Foster grant opportunities in Aboriginal and Torres Strait Islander health research that are:
- Co-designed with community and Aboriginal and Torres Strait Islander researchers.
- Embed processes that enable research to be successfully undertaken in community settings, such as the length of time and funding that is required to build relationships.
- Adopt consistent approaches/criteria for researchers that outlines community leadership through genuine partnerships with relevant Aboriginal community organisations.
Why we should do it
Positive results are seen when Aboriginal and Torres Strait Islander research is strengths-based and undertaken utilising the principles of self-determination and equity.54–56 Aboriginal and Torres Strait Islander researchers have continued to call for grant processes to align with community needs, particularly taking into account the time and resources required to mobilise research in community settings.57
What it could achieve
- More targeted priority setting processes with greater visibility and transparency for research that is led by Aboriginal and Torres Strait Islander researchers.
- Understanding areas that are being appropriately funded and areas of unmet need that may require greater resourcing.
- Identification of potential synergies across funders for consolidated funding opportunities that could achieve more impactful outcomes through collaborative projects and networks.
- Processes that are more aligned to the needs of the community, leading to better research outcomes that are easier to translate into policy and practice.
- More projects designed with community and genuine partnerships among researchers and community.
Lowitja Institute’s research grants program58
 Lowitja Institute is Australia’s only Aboriginal and Torres Strait Islander community controlled health research institute. As a commissioning body, Lowitja Institute’s research is built on key priorities identified by Aboriginal and Torres Strait Islander peoples, which aims to produce high impact research, tools and resources that will have positive health outcomes for Australia’s First Nations. Lowitja Institute facilitates engagement between Aboriginal and Torres Strait Islander communities, tertiary education, medical research institutions, government, and partner organisations to maximise the impact of research, knowledge and innovation. By funding only Aboriginal and Torres Strait Islander community controlled organisations and researchers, the Lowitja Institute is actively strengthening the Aboriginal and Torres Strait Islander research workforce. Major research grants support innovative and responsive research with additional funding provided for knowledge translation activities. Seeding grants support the scoping of community research priorities and engage translational research partners to co-create meaningful research projects.
Lowitja Institute is Australia’s only Aboriginal and Torres Strait Islander community controlled health research institute. As a commissioning body, Lowitja Institute’s research is built on key priorities identified by Aboriginal and Torres Strait Islander peoples, which aims to produce high impact research, tools and resources that will have positive health outcomes for Australia’s First Nations. Lowitja Institute facilitates engagement between Aboriginal and Torres Strait Islander communities, tertiary education, medical research institutions, government, and partner organisations to maximise the impact of research, knowledge and innovation. By funding only Aboriginal and Torres Strait Islander community controlled organisations and researchers, the Lowitja Institute is actively strengthening the Aboriginal and Torres Strait Islander research workforce. Major research grants support innovative and responsive research with additional funding provided for knowledge translation activities. Seeding grants support the scoping of community research priorities and engage translational research partners to co-create meaningful research projects.
Network Environments for Indigenous Health Research (NEIHR)59
 In 2018, the NEIHR program was launched by the Canadian Institutes of Health (CIHR). The NEIHR program is led by the Institute of Indigenous Peoples' Health, co-led by the Institute of Circulatory and Respiratory Health and financially supported by all 13 CIHR institutes. The NEIHR program has set the foundation for establishing a national network of centres focused on strengthening Indigenous research capacity, training and mentoring, and supporting Indigenous community-based health research that reflects the priorities and values of Indigenous Peoples.
In 2018, the NEIHR program was launched by the Canadian Institutes of Health (CIHR). The NEIHR program is led by the Institute of Indigenous Peoples' Health, co-led by the Institute of Circulatory and Respiratory Health and financially supported by all 13 CIHR institutes. The NEIHR program has set the foundation for establishing a national network of centres focused on strengthening Indigenous research capacity, training and mentoring, and supporting Indigenous community-based health research that reflects the priorities and values of Indigenous Peoples.
Translation and implementation
Prioritise community based, innovative solutions to implement research outcomes that address the National Agreement on Closing the Gap.
How we could do it
- Better coordinate research and translation activities with ‘Closing the Gap’ targets by:
- Working with funders to ensure funding opportunities are clearly linked to ‘Closing the Gap’ priority areas, particularly areas that require further attention.
- Encouraging processes among funders to better identify how all health and medical research improves the health and wellbeing of Aboriginal and Torres Strait Islander peoples – a process currently being piloted by the NHMRC.60
- Closer monitoring of research activity and its contribution to progress on ‘Closing the Gap’ by working with agencies such as the Productivity Commission, the Lowitja Institute and other key Aboriginal and Torres Strait Islander health research organisations, including ACCHOs.
- Continue to grow investment in RTCs that focus on Aboriginal and Torres Strait Islander Health and work across Commonwealth, state and territory funders to build translation incentives into funding mechanisms.
- Design grant opportunities that focus on the translation and implementation of research by including a requirement to clearly articulate a feasible translation pathway, evidence of genuine partnerships with community and alignment with existing frameworks. Implement processes so funding agencies can monitor translation of funded projects to inform future grant opportunities.
- Design better mechanisms of sharing research and translation outcomes through networks and data sharing portals that can be easily accessed by researchers, funders and policymakers (see Focus Area 1 Collaborative platforms and networks).
Why we should do it
Investment in Aboriginal and Torres Strait Islander health research has increased. It is now time to set processes in place to monitor and evaluate the impact of this research on the health and wellbeing of Aboriginal and Torres Strait Islander Peoples, and progress towards the ‘Closing the Gap’ targets, to inform future funding decisions.
What it could achieve
- Improved health and wellbeing outcomes in the Aboriginal and Torres Strait Islander community through projects that are designed with feasible translation and implementation pathways.
- Leveraging effective elements of the Research Translation Centres
- Greater visibility of research achievements and translation outcomes, to reduce duplication and improve the design of new funding opportunities and research projects.
- Better alignment of health and medical research to ‘Closing the Gap’ targets.
Kimberley Aboriginal Health Research Alliance (KAHRA)61
 KAHRA brings together Kimberley health services, Aboriginal communities and research organisations to fundamentally change how research is designed, conducted and used in the Kimberley. This collaboration combines the wisdom and cultural strength of communities, the knowledge and commitment of regional health services and research expertise to drive evidence-based change. The activities of KAHRA are intended to ‘flip’ the state of investigator-driven research to instead have communities and health services directly driving the research agenda, for better health outcomes for Kimberley Aboriginal people.
KAHRA brings together Kimberley health services, Aboriginal communities and research organisations to fundamentally change how research is designed, conducted and used in the Kimberley. This collaboration combines the wisdom and cultural strength of communities, the knowledge and commitment of regional health services and research expertise to drive evidence-based change. The activities of KAHRA are intended to ‘flip’ the state of investigator-driven research to instead have communities and health services directly driving the research agenda, for better health outcomes for Kimberley Aboriginal people.
Central Australian Academic Health Science Network (CAAHSN)62
 Researcherenye Wappayalawangka - CAAHSN is an RTC accredited by the NHMRC. Researcherenye is an Arrernte rendering of a borrowed word describing a gathering of researchers. Wappayalawangka is made up of the first one or 2 letters of the 14 First Nation languages represented in central Australia.
Researcherenye Wappayalawangka - CAAHSN is an RTC accredited by the NHMRC. Researcherenye is an Arrernte rendering of a borrowed word describing a gathering of researchers. Wappayalawangka is made up of the first one or 2 letters of the 14 First Nation languages represented in central Australia.
The network is dedicated to improving the health of people in central Australia, with a focus on Aboriginal health. It is focused on community driven research and research translation in close collaboration with research, educational and service delivery organisations.
Aboriginal and Torres Strait Islander leadership and workforce capacity and capability building
Enhance Aboriginal and Torres Strait Islander health and medical research leadership and support emerging researchers in innovative cross-disciplinary fields, particularly community-based researchers with non-traditional pathways into research.
How we could do it
- Increase understanding of the profile of the Aboriginal and Torres Strait Islander health and medical research workforce as part of the wider Australian Health and Medical Research Workforce Plan (see Workforce Enabling Initiative).
- Ensure there is sustained and sufficient investment in existing networks (e.g OCHRe) and for initiatives from the Lowitja Institute and ACCHOs that are having a positive impact in growing and developing the Aboriginal and Torres Strait Islander research workforce.
- Invest in innovative, cross-disciplinary health and medical research led by Aboriginal and Torres Strait Islander researchers and training programs to build skills in areas of translation, commercialisation and implementation science including as part of undergraduate and postgraduate degrees.
- Increase Aboriginal and Torres Strait Islander leadership and capacity building educational pathways to support the development of future Aboriginal and Torres Strait Islander health and medical researchers (e.g. micro-credentials and fellowships).
- Appropriately acknowledge the experiences and diverse backgrounds of community-based researchers in the review of grant applications.
- Ensure community-based researchers receive fair recognition on research outputs through appropriate guidelines.
Why we should do it
Building the Aboriginal and Torres Strait Islander researcher workforce provides opportunities to incorporate Aboriginal and Torres Strait Islander knowledges for innovative solutions to complex problems. Community-based researchers have an in-depth understanding of the issues that are important for the community. Growing the workforce will also relieve some burdens carried by the current workforce who face multiple demands and unique challenges.
What it could achieve
- A better understanding of the stories, settings, demographics and career paths of past and current Aboriginal and Torres Strait Islander researchers so the National Strategy can elevate policies to reduce barriers to workforce entry and continue to build capacity and capability.
- Ongoing funding and resourcing of successful networks that ensures achievements to date will continue and grow.
- More innovative solutions and greater cross-disciplinary training for Aboriginal and Torres Strait Islander people that is needed to ‘Close the Gap’ and deliver better outcomes for the community.
- Alignment of organisations that share a common goal to advance the future Aboriginal and Torres Strait Islander workforce through education and employment opportunities.
- Acknowledgment of the diverse experiences of community-based researchers (so often different to other academic researchers) to ensure grant applications are reviewed and assessed equitably.
- Appropriate attribution of community-based researchers in research outputs as an important measure of research productivity, which will also aid the development of more diverse research careers.
Our Collaborations in Health Research (OCHRe)63
 OCHRe is a national network of First Nations researchers that support a culturally secure and inclusive research network. OCHRe plays a key role in developing the next generation of First Nations research leaders by providing a supportive, connected environment. It represents the largest group of Indigenous researchers brought together under a single NHMRC application, ensuring First Nations perspectives are central to shaping Australia’s health research. OCHRe builds on the unique skills at the interface of Indigenous knowledges, science and health research with the aim of improving the health and wellbeing of Aboriginal and Torres Strait Islander Peoples.
OCHRe is a national network of First Nations researchers that support a culturally secure and inclusive research network. OCHRe plays a key role in developing the next generation of First Nations research leaders by providing a supportive, connected environment. It represents the largest group of Indigenous researchers brought together under a single NHMRC application, ensuring First Nations perspectives are central to shaping Australia’s health research. OCHRe builds on the unique skills at the interface of Indigenous knowledges, science and health research with the aim of improving the health and wellbeing of Aboriginal and Torres Strait Islander Peoples.
OCHRe initiatives are many and the following are a few examples:
- Research Experience Scholarships for non-research degree students
- Travel scholarships to attend academic forums and conferences
- Professional development research workshops for clinicians
- Education and training of students in a Certificate IV in Aboriginal and Torres Strait Islander Research Theory and Practice
- Developing an Indigenous Knowledges and Cultural Safety Frameworks
- Genomics Our Way – online course ‘An Introduction to Genomics Research with Indigenous Australians’
Focus area 4: Drive impact through research translation, innovation and commercial solutions
Overview
Mechanisms that incentivise and support research translation, commercialisation and industry growth will deliver economic gains, a robust biotech and medtech sector and health system capability, resilience and future preparedness.
| Drive national prosperity and security | Advancing health and medical research innovation, translation and commercialisation will drive national prosperity and security by fostering investment and improving health outcomes. |
|---|---|
| Lead the world in health outcomes | More rapidly translating research findings into innovative policy, practice and products will enable Australia to deliver world leading health outcomes. |
| Deliver equity – no one left behind | Australia’s diverse health system, together with research underpinned by Open Science principles, will help to ensure that all communities benefit from the rapid translation of research and innovations into high value care. |
| Secure a resilient and sustainable health system | Enhancing research translation will support improved access to novel treatments and care, while building sovereign innovation and commercialisation will support resilience in the face of future health challenges. |
| Strengthen regional and global partnerships | Australia’s capacity to translate and scale up research quickly and effectively will provide a platform to develop and enhance partnerships that improve health outcomes, regionally and globally. |
Research translation
Strengthening organisational structures, policies, funding models and performance indicators to promote research-positive cultures will foster meaningful collaboration between researchers, clinicians and the community. These collaborations will embed research and translation expertise – particularly for regional, rural, remote and other underserved communities – and improve patient outcomes. At the same time, developing clear pathways for the validation, scaling and widespread uptake of evidence-based prevention and population health innovations will enhance efficiency and equity of the health system overall.
Industry integration and risk sharing
Identifying and implementing programs to share risk and harmonise regulatory, approval and procurement pathways will help drive industry investment and growth. These programs will build sovereign capability in the production and manufacture of medical diagnostics, devices and pharmaceuticals. In addition, increasing opportunities for research-industry exchanges, training and alternative career pathways for researchers will help to bridge academia and business. This will ensure Australia has the workforce it needs to support a strong and broad-based biotech and medtech sector into the future.
Manufacturing and marketing
Building on existing strategies and models to enhance Australia’s biotech and medtech manufacturing and marketing capacity will enable an increase in local production and export of Australian products to global markets. Focusing on building skills, expertise and collaboration from discovery research to market will strengthen Australia's health system and deliver benefits to the community and broader economy.
In a LHS, research, data and practice are systematically and continuously integrated to improve patient outcomes and provide high value, cost efficient care.
Key characteristics of a LHS include real time access to knowledge and healthcare data; strong and meaningful patient-clinician partnerships; incentives to encourage value-based care; organisational leadership and systems that support research- and learning-positive cultures; and policies, governance and regulations that are aligned to facilitate research, collaboration, and learning.64
Developing, supporting and enhancing LHS models in all healthcare delivery settings is key to advancing research translation, improving evidence-based care delivery and supporting system efficiency. A LHS requires a range of supporting stakeholders to work together in ways that are context-specific, relevant and meaningful. For the Australian healthcare system these stakeholders include Commonwealth, state and territory government agencies, policy makers, healthcare administrators, professional training and accreditation and peak bodies, and collaborative networks of practitioners, consumers and the community.
Research translation
Develop and expand on current structural solutions and initiatives, such as RTCs and hub and spoke models, to embed translation and research expertise in healthcare settings.
How we could do it
- Continue to support and expand the operation of RTCs, especially those with a specific focus on Aboriginal and Torres Strait Islander, regional, rural and remote and underserved populations, harnessing the professional development support they can provide for clinician researchers.
- Leverage the work of other research translation initiatives underway in private practice, and across state, territory and local jurisdictions, acknowledging the importance of the specific needs of different communities and valuing differences of approach to the overall goal of improving health.
- Establish incentives and support mechanisms for public health, hospitals and health networks to embed LHS models that will grow research-positive cultures and systems, improve patient outcomes and provide high value, cost efficient care.
- Embed performance indicators for research within healthcare settings into existing funding arrangements to enhance implementation of research activity.
Why we should do it
- Accredited Australian RTCs have delivered benefits at both the community and national level by providing a base for local networks to drive implementation of research into practice and achieve better patient outcomes at the community level. RTCs also facilitate the sharing of expertise and experience at the national level. As currently configured RTCs are primarily place based. New opportunities exist to build on and expand the model to support broader translation initiatives for even greater impact.
- While Australia has made substantial investments in supporting research translation, widespread implementation of research findings and evidence-based prevention, treatment and therapeutic innovations remains a significant challenge, particularly for RRR areas, Aboriginal and Torres Strait Islander health and underserved communities.
- There is evidence for the effectiveness of hub and spoke models that decentralise and extend translational activities and enable collaboration into a variety of settings, for example, teletrial designs that extend resources and upskill health care organisations into rural and remote areas.65
What it could achieve
- More research projects implemented in health services.
- Increased delivery of high value, evidence-based care in healthcare settings.
- Greater impact of research, with more research moving into practice, improving patient outcomes and health system efficiency.
- Increased consumer and community engagement, aided by RTCs, embedding lived experience in all stages of the research endeavour.
- Increased research-intensive Australian healthcare services, regardless of where they are or the communities they serve.
- Development of training programs for the next generation of clinician-researchers, implementation scientists, and community partners.
The Australian Health Research Alliance (AHRA)66
 AHRA represents 12 NHMRC accredited and 2 emerging RTCs operating across all states and territories. Collectively AHRA comprises 169 partners including health services, universities, research institutes and community organisations.
AHRA represents 12 NHMRC accredited and 2 emerging RTCs operating across all states and territories. Collectively AHRA comprises 169 partners including health services, universities, research institutes and community organisations.
Each RTC operates independently to pursue research priorities and work programs relevant to the communities in which they operate. They also collaborate and share their collective expertise in support of the overall mission to support health and medical research to be translated and embedded into healthcare to improve health outcomes, health equity and the health economy.
Examples of National System Level Initiatives coordinated through the AHRA network include a program of work aimed at embedding consumers in health research policy and practice, a Women’s Health Research Translation Network to boost national and international collaboration on women’s health and research, negotiation of Data Sharing Accords between partners to facilitate access to health data for research use, and a National Indigenous Research(er) Capacity Building Network to support and grow the next generation of Indigenous researchers working in Aboriginal and Torres Strait Islander health.
Industry integration and risk sharing
Establish mechanisms that optimise research-industry exchange and moderate and share risk for industry to stimulate investment attractiveness, build sovereign capability and drive commercial outcomes.
How we could do it
- Consolidate and leverage existing research and development (R&D) funding and support initiatives to provide targeted, fit for purpose support for different health and medical products, modalities or interventions, with a focus on supporting innovators and startups at the early stages of development and commercialisation.
- Identify gaps and solutions to streamline regulatory pathways and reduce time to market.
- Work across government and with industry to identify optimal ways to support high-risk, high-reward innovation in strategically important areas of R&D where market conditions or capital constraints preclude private investment.
- Encourage and reward researcher movement across discipline and sector boundaries, including through translational fellowships and industry PhDs, to strengthen the bridge between academia and business.
- Enhance opportunities for Aboriginal and Torres Strait Islander capability building in entrepreneurship and commercialisation to support the growth of community led industries.
- Support the SERD process in mapping where government and industry action can make the greatest impact on health and medical research commercialisation to increase Australia’s market competitiveness.
Why we should do it
- More than 80% of Australian biotech and medtech companies are small and medium enterprises working in the early stages of translating research into commercial products.67
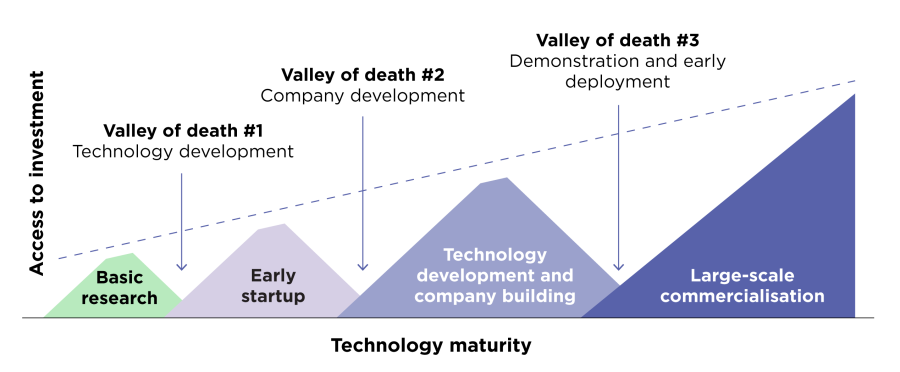
- Companies face significant challenges moving through the ‘valleys of death’ from early stage research to large scale commercialisation (it can take 7–15 years and up to $2.5 billion to bring one biomedical product from early research to market).67
- Access to capital is cited by businesses as the number one barrier to commercialisation in Australia.68
- Australian companies continue to struggle to secure skilled staff – in 2021, MTPConnect identified key skills gaps across critical areas such as business operations, health economics and regulatory affairs, health data and cyber security.69
What it could achieve
- Increased industrial capacity and capabilities.
- Increased investment in Australian startups and small to medium enterprises (SMEs).
- Increased local R&D presence of biotech and medtech multinationals in Australia.
MTPConnect470
 MTPConnect was established by the Australian Government as an independent, not for profit organisation to support the growth of the Australian medical products sector.
MTPConnect was established by the Australian Government as an independent, not for profit organisation to support the growth of the Australian medical products sector.
MTPConnect improves collaboration and commercialisation, funding cutting edge innovations, improving management and workforce skills, optimising the regulatory and policy environment and improving access to global supply chains and strategic international markets. A significant number of MTPConnect’s programs and funding opportunities are offered in partnership with the federal government, particularly MRFF initiatives, and state governments. MTPConnect also regularly collaborates with sector organisations and peak groups like Medicines Australia, MTAA and AusBiotech, and trade agencies including Austrade to deliver programs and advocate on behalf of the biotech and medtech sector.
European Innovation Council (EIC)71
The EIC has been established under the EU Horizon Europe program to support innovation throughout the lifecycle from early stage research to proof of concept, technology transfer, and the financing and scale up of startups and SMEs. EIC provides funding for individual companies (mainly startups and SMEs) through both grants and investments in the form of direct equity or quasi-equity investments managed by the EIC Fund.
Manufacturing and marketing
Support commercialisation and sovereign capability by building local biotech and medtech manufacturing and industry marketing capabilities and research-industry partnerships for national and international markets.
How we could do it
- Establish a central platform to provide consolidated, consistent and up to date information on intellectual property and commercialisation funding initiatives, training and support programs available for Australian innovators at all stages of the commercialisation pathway.
- Support and assist the actions outlined in the Medical Science Co-investment Plan72 for increasing industrial capacity and capabilities, supporting the commercialisation of high value products, and improving the international competitiveness of the Australian medical science and technology sector.
- Prioritise the development of sovereign capability and supply chain resilience by encouraging and incentivising local procurement of medical products where feasible.
- Continue to build on the innovation precinct model as a mechanism for embedding links between universities, hospitals, startups, and manufacturers that build expertise and capacity to manage and develop intellectual property across the entire value chain, from discovery research to manufacture and marketing.
Why we should do it
- Manufacturing capacity, streamlined regulatory pathways and access to national and international markets are key to securing sovereign capability, economic resilience and the growth of Australia’s biotech and medtech future.
- Limited access to a small number of local research and manufacturing facilities presents challenges to Australian innovators.73
- Over 90% of prescription medicines and 97% of all diagnostic raw materials and components are imported into Australia.74
- The Australian biotech and medtech sector is maturing and developing the key prerequisites for successful biotech and medtech precincts: infrastructure, access to skills, capital and market know-how; enterprise culture; positive regulatory and governance conditions; and competitive advantage.75
What it could achieve
- More Australian made biotech and medtech products used in Australian healthcare and exported internationally, generating financial benefits and economic growth.
- Faster access to innovative therapies for Australian patients and faster response to health emergencies, including pandemics and antimicrobial resistance.
- Reduced reliance on imports for critical medicines, vaccines, diagnostics and biologics.
- Improved health equity through locally produced, affordable technologies.
- Expansion of Australian biotech and medtech industries into local and international markets.
ADAPT®76
 Australian healthcare company, Admedus Limited, in collaboration with West Australian heart researcher and inventor Professor Leon Neethling, developed the ADAPT® tissue engineering process which transforms animal tissue into durable bioscaffolds that can be used to mimic human tissue for surgical repair (Cardiocel®).
Australian healthcare company, Admedus Limited, in collaboration with West Australian heart researcher and inventor Professor Leon Neethling, developed the ADAPT® tissue engineering process which transforms animal tissue into durable bioscaffolds that can be used to mimic human tissue for surgical repair (Cardiocel®).
Originally produced in small batches at Royal Perth Hospital, Admedus opened a manufacturing facility in 2014 in Malaga, WA to support broader surgical use, particularly in babies and children with heart defects. ADAPT® tissue has since been distributed for use in over 55,000 patients globally.
In 2022, Admedus changed its name to Anteris Technologies and pivoted to a structural heart company. The novel acellular, biostable and non-calcifying ADAPT® tissue was molded into a single-piece 3D biomimetic heart valve (DurAVR® THV) with excellent early clinical results in the treatment of severe aortic stenosis, a life-threatening condition. A global study to commercialise the DurAVR® transcatheter heart valve will commence this year.
Focus area 5: Position to be ready for future needs and challenges
Overview
Knowledge exchange and harnessing AI will ensure Australia has capacity, trust in science and sovereign capability to monitor and address global risks and opportunities. This capability will support Australia to face future health and environmental challenges and to be a strong contributor to global and regional partnerships.
| Drive national prosperity and security | Ensuring Australia is prepared for future needs and challenges, and has the capacity to respond, will advance national prosperity and resilience, contributing to national security. |
|---|---|
| Lead the world in health outcomes | Being prepared for future needs and challenges empowers Australia to continue to contribute as a global and regional leader in achieving outstanding health outcomes. |
| Deliver equity – no one left behind | Applying an equity lens to emerging technologies, environmental sustainability, and global partnerships will enable inclusive planning that leaves no one behind. |
| Secure a resilient and sustainable health system | Strengthening preparedness for future needs and challenges plays a vital role in building a resilient and sustainable health system, that is fit for purpose and able to adapt. |
| Strengthen regional and global partnerships | Australia’s strengths in health and medical research underpin a leadership role in addressing global and regional health challenges. |
Emerging technology
Building capability in emerging technologies is essential for a high performing health and medical research ecosystem. These technologies ensure that research remains fit for purpose, responsive to future challenges and well positioned to seize new opportunities.
Innovations such as gene and cell therapies and genomic medicine hold transformative potential for addressing some of Australia’s most pressing health issues. In parallel, advances in therapeutic approaches, AI and digital health play an increasingly critical role in drug discovery, diagnostics, clinical decision-making and enhancing healthcare delivery and access.
AI and digital health tools can further improve healthcare outcomes by streamlining clinical workflows, supporting patient engagement, promoting equitable access and advancing health literacy across diverse populations.
Environmental sustainability
Integrating environmentally sustainable practices into research design, infrastructure and operations reduces the ecological footprint of research and aligns with broader public health goals.
By adopting sustainable procurement practices, minimising waste and investing in green technologies, the research community can lead by example – demonstrating that scientific advancement and environmental stewardship can go hand in hand. This approach supports long term health outcomes by protecting the ecosystems that underpin community wellbeing.
Global partnerships
Global partnerships are vital to advancing health and medical research, sharing knowledge and expertise across borders. In an increasingly interconnected world, health challenges such as pandemics, antimicrobial resistance, chronic and rare diseases require coordinated, collaborative responses that no single country can address alone. Collaboration accelerates scientific discovery, facilitates access to diverse populations and data sets and supports the development of globally relevant solutions. Strengthening these partnerships enhances resilience, innovation and preparedness for future needs and challenges.
Open science, trust in science and effective regulation are foundational to the integrity and impact of health and medical research.
These elements of the health and medical research ecosystem ensure that scientific findings are accepted, acted upon, and translated into improved health outcomes. They foster a research environment that is transparent, accountable and responsive to societal needs, ultimately strengthening the credibility and utility of scientific advancements in health and medicine.
Emerging technology
Build capability and capacity to take advantage of innovative emerging technologies including cutting edge approaches for responsible and impactful harnessing of AI.
How we could do it
- Harness AI capabilities, advanced technology infrastructure and manufacturing capabilities for health and medical research through a nationally coordinated policy approach. This will be achieved by aligning efforts across jurisdictions and with industry to build an integrated ecosystem to support cutting edge research, accelerate technology adoption and strengthen domestic production capabilities.
- Define and implement policy frameworks that give appropriate protections for sensitive and valuable health and medical research data. These frameworks will address data governance, privacy, security and ethical use, to enable responsible data sharing and collaboration across jurisdictions.
- Engage with international horizon scanning initiatives to proactively identify and leverage emerging technologies and AI in health and medical research.
Why we should do it
- Advanced technologies and AI are rapidly evolving, presenting both opportunities and challenges for the health system and research environment. It is important that the Australian health system adapts to take advantage of the benefits of AI, while balancing necessary protections to ensure safety and privacy.
- It is estimated that globally, AI in the healthcare market is expected to reach USD67.4 billion by 2027, growing at a compound annual growth rate of 46%.77
- The Commonwealth and many states and territories have or are implementing health identifiers and digital patient records. Digital technologies are easing pressure on health services and, through data sharing, informing evidence-based decision making.
- Australians, as early adopters, are already on track to embrace emerging technologies. The National Digital Health Survey (2021)78 revealed consumers intend to increase their use of digital health in the future for self-servicing tasks such as booking healthcare appointments online or accessing electronic health records and prescriptions.
- Embedding digital technologies offers advantages for health services, such as:
- Real time access to patient health data and information across different healthcare settings and borders, to support immediate, evidence-based clinical decision making;
- providing patients with access and control of their own health data;
- distributing digitally enabled patient screening and medication alerts; and
- generating data-driven insights for better practice planning, resourcing and continuous quality improvements.
- Despite the benefits, Australians are not yet equitably benefiting. Health providers and consumers have differing access to, and experience with, current and emerging digital technologies.
What it could achieve
- Position Australia as a global leader in AI and innovation, accelerating the translation of cutting edge research into practical applications.
- A secure and interoperable data environment supporting innovation while safeguarding public trust.
The Centre for Health Record Linkage (CHeReL)79
CHeReL links multiple sources of data and maintains a record linkage system that protects privacy. This allows for an accurate and more complete picture of the health of the population to be provided. CHeReL has contributed to the capacity of researchers to access linked data from across many different datasets through probabilistic linkage.
The Singapore Integrated Diabetic Retinopathy Programme (SiDRP)80
SiDRP is a 12 year research and translation platform investment by government to link in real time digital retinal images from all the nation’s 23 polyclinics to the Singapore National Eye Centre. AI has enhanced early detection of diabetic retinopathy, establishing the world's first nationwide AI-driven disease screening system. This approach is estimated to deliver cost savings of SGD144 per patient over the traditional family physician model.
Environmental sustainability
Consider the impact of health and medical research and health system outcomes on climate as a key factor in priority setting to embed research processes that promote environmental sustainability.
How we could do it
- Embed targeted policy initiatives and cross-sector engagement to reduce the environmental impacts of health and medical research by communicating and promoting the benefits of modern, responsive and adaptable research practices that improve environmental impacts of research on people, organisations and society.
- Consider the impact of health and health system outcomes on climate change, as a focus of research priority setting processes.
- Incorporate Aboriginal and Torres Strait Islander knowledge systems, innovations and practices into sustainable health and medical research practices, through engagement and co-design.
Why we should do it
- People in Australia are experiencing the impacts of climate change on their health. The increasing frequency, intensity and duration of extreme weather events is leading to more deaths, disease and injury, and adversely impacting mental health and wellbeing.81
In 2023, the Australian Government launched the first ever National Health and Climate Strategy,82 with 4 core objectives:
1. health system resilience;
2. health system decarbonisation;
3. international collaboration;
4. health in all policies.
Consistent with these objectives, Australian health and medical research can support health, climate-resilient and sustainable communities through the work practices of the health and medical research ecosystem.
- International funders of health and medical research are implementing progressive policies and commitments to environmental responsibility.
What it could achieve
- Recognising and mitigating environmental impact across all facets of health and medical research as an integral part of research culture.
- Prioritising research into health and health system impacts of climate change and how these challenges can be addressed going forward.
- Adopting sustainability adopted as a core research ethic, including by incorporating generations of Aboriginal and Torres Strait Islander knowledge and practices.
Tasmanian Department of Health
Tasmania has a net zero target for greenhouse emissions by 30 June 2030.83 In support, the Tasmanian Department of Health developed and released a 2019 framework for action focused on establishing a sustainable health unit, reducing emissions, sustainable food choices and new delivery models, including reducing unnecessary medical tests and treatments.84
The Australian Commission on Safety and Quality in Health Care (ACSQHC)
ACSQHC in partnership with the Australian Centre for Disease Control (ACDC) and the Australian Medical Colleges released a joint statement in 2024 signifying a shared commitment to address the health impacts of climate change.85 The Working together to achieve sustainable high quality health care in a changing climate statement recognises the challenges of climate change, and the risks posed to physical and mental health.
UK National Institute for Health and Care Research (NIHR)
NIHR’s commitments to climate, health and sustainability 2024–202686 include:
- publishing a baseline of their carbon footprint and developing an action plan to reduce it;
- increasing funding for climate, health and sustainability research, including research to protect human health, and research to help the healthcare system become more sustainable.
Wellcome Trust
The Wellcome Trust (UK) has played a key role in developing a Concordat for the Environmental Sustainability of Research & Innovation Practice,87 which commits signatories to ensuring research and innovation they undertake or fund is practiced in an environmentally sustainable way. The Concordat currently has more than 75 signatories who agree to take institutional action to reform leadership and system change, sustainable infrastructure and procurement, emissions from business and academic travel, advocating through collaborations and partnerships and transparent reporting of environmental impact.
Global partnerships
Promote strategic collaborations that address shared health priorities to strengthen Australia’s leadership globally and in the Indo-Pacific region.
How we could do it
- Work to define global health and health security as issues of high priority to Australia and regional neighbours. Identifying and addressing trans-boundary health threats that are a risk to national and regional stability will allow health system strengthening, surveillance programs and preparedness policies to be developed in collaboration with global and regional partners.
- Support pathways of collaboration, capacity strengthening and knowledge exchange to draw on international expertise aligned with Australian priorities. This will be achieved through enduring bilateral and multilateral relationships and agreements.
Why are we doing it
- Regional partnerships are critical to improve health security and to develop and implement solutions for disease prevention, treatment and emergency response to global health challenges.
- There is already a high level of international engagement of Australian health and medical researchers:
- International mobility is particularly common among health and medical researchers, with 35% moving to Australia for a research job and 44% having worked overseas at some point in their careers.88 This mobility and engagement enhances Australia's participation in global scientific networks and collaboration.
- At the global level, the share of publications representing international collaboration has increased from 4.7% in 1980 to 25.7% in 2021.89
- Strategic collaborations towards internationally shared health priorities aligns with the Commonwealth’s Medical Science Co-investment Plan72. The Plan aims to capture more value from Australia's world leading medical science sector by increasing industry capability and capacity, supporting commercialisation and improving our international competitiveness.
What it could achieve
- Strengthening Australia's position as a global contributor to positive health outcomes.
- Increased leadership roles for Australia in regional health governance and strategic investment, coordinating action that addresses health threats and priorities across borders.
- Increased capacity of our regional and global partners to address complex health and medical research challenges arising from Australian engagement and partnerships.
Partnerships for a Healthy Region
Part of Australia’s continued investment in the health of our region, this initiative is an important contribution to the Pacific and Southeast Asia’s recovery from COVID-1990. It aims to help build resilient and equitable health systems in the Pacific and Southeast Asia to reduce disease risks and burdens, and uplift effective responses to health emergencies. Investments under the Partnerships contribute to:
- Communicable disease prevention and control.
- Non-communicable disease prevention and control.
- Sexual and reproductive health and rights.
- Resilient health systems.
- Effective partnerships and delivery.
Elimination Partnership in the Indo-Pacific for Cervical Cancer (EPICC)91,92
EPICC leverages expertise across Australia and globally to accelerate the WHO’s strategy for the elimination of cervical cancer. Partnering with local and international organisations, EPICC promotes HPV vaccination, screening, and treatment and has made global impact on women's lives.
References
12 Waltman L, Rafols I, van Eck NJ and Yegros A (2019). Supporting priority setting in science using research funding landscapes. RoRI Working Paper No.1, Research on Research Institute. London: Research on Research Institute. doi.org/10.6084/m9.figshare.9917825
13 Australian Council of Learned Academies (ACOLA). Horizon Scanning Series: An overview acola.org/our-work/horizon-scanning-series/ (accessed 16 July 2025).
14 Lapham K, Fox N, Goddard S. (2024). Horizon Scanning in the New Zealand Health System. Commissioned by Medicines New Zealand Biointelect. www.biointelect.com/horizon-scanning-in-the-new-zealand-health-system/ (accessed 16 July 2025).
15 Australian Institute of Health and Welfare (2024). Health promotion and health protection. Retrieved from www.aihw.gov.au/reports/australias-health/health-promotion (accessed 22 August 2025).
16 WHO guidance on the ethics of health research priority setting. Geneva: World Health Organization; 2025. Licence: CC BY-NC-SA 3.0 IGO. iris.who.int/bitstream/handle/10665/381711/9789240110953-eng.pdf (accessed 16 July 2025).
17 Centre for Epidemiology and Evidence (2023). Setting Research Priorities: A Guide. Evidence and Evaluation Guidance Series, Population and Public Health Division. NSW Ministry of Health.
18 The James Lind Alliance Guidebook, Version 10 (2021). National Institute for Health and Care Research www.jla.nihr.ac.uk/jla-guidebook (accessed 16 July 2025).
19 Horizon scanning and landscape assessment. World Health Organisation. www.who.int/our-work/science-division/research-for-health/optimizing-research-processes/landscape-assessment (accessed 16 July 2025).
20 The interim Australian Centre for Disease Control (CDC). www.cdc.gov.au/ (accessed 21 August 2025)
21 RNA Production and Research Network. New South Wales Health and Medical Research. www.medicalresearch.nsw.gov.au/nsw-rna-production-and-research-network/ (accessed 16 July 2025).
22 Bioplatforms Australia: Advancing life science through biomolecular infrastructure and national collaboration. bioplatforms.com/ (accessed 16 July 2025).
23 Department of Health, Disability and Aged Care (2025). Report on findings from the National Health and Medical Research Community Qualitative Research. www.health.gov.au/resources/publications/report-on-findings-from-the-national-health-and-medical-research-community-qualitative-research?language=en (accessed 16 July 2025).
24 Australian Institute of Health and Welfare (2025). Rural and Remote Health. www.aihw.gov.au/reports/australias-health/rural-and-remote-health (accessed 2 June 2025).
25 Consultation summary report: Improving alignment and coordination between the Medical Research Future Fund and NHMRC’s Medical Research Endowment Account (2024). www.health.gov.au/sites/default/files/2024-05/consultation_summary_report_-_improving_alignment_and_coordination_between_the_mrff_and_nhmrc_mrea.pdf (accessed 16 July 2025).
26 NHMRC Leadership and Governance. Committees. www.nhmrc.gov.au/about-us/leadership-and-governance/committees (accessed 16 July 2025)
27 UK Research and Innovation (UKRI). https://www.ukri.org/who-we-are/ (accessed 9 July 2025)
28 Willson ML, Seidler AL, Aberoumand M, Williams JG, Hunter KE, Barba A, Webster AC, Askie LM, Simes RJ. (2022). Latest update of the clinical trials landscape in Australia 2006 – 2020. Sydney: Australian New Zealand Clinical Trials Registry. doi.org/10.25910/t9n1-bm45
29 Australian Clinical Trials Alliance (2020). Clinical trial awareness and access amongst culturally and linguistically divers (CALD) populations: environmental scan. clinicaltrialsalliance.org.au/wp-content/uploads/2020/06/ACTA-Clinical-trials-and-CALD-population_Environmental-Scan-V3_final.pdf (accessed 16 July 2025)
30 The Sex and Gender Sensitive Research Call to Action Group (2020). Sex and gender in health research: updating policy to reflect evidence. Med J Aust 2020, Vol 212, No. 2, pp 57-62. doi: 10.5694/mja2.50426
31 Waltz M, Lyerly AD and Fisher JA (2023). Exclusion of Women from Phase I Trials: Perspectives from Investigators and Research Oversight Officials. Ethics & Human Research, Vol 45, No. 6, pp 19-30. doi: 10.1002/eahr.500170
32 Department of Health and Aged Care and NHMRC (2024). Statement on Sex, Gender, Variations of Sex Characteristics and Sexual Orientation in Health and Medical Research. www.nhmrc.gov.au/research-policy/gender-equity/statement-sex-and-gender-health-and-medical-research (accessed 16 July 2025)
33 Australian Clinical Trials Alliance. Economic evaluation of investigator-initiated clinical trials conducted by networks. Sydney: ACSQHC; 2017. www.safetyandquality.gov.au/publications-and-resources/resource-library/economic-evaluation-investigator-initiated-clinical-trials-conducted-networks-final-report (accessed 17 July 2025)
34 Breast Cancer Trials. www.breastcancertrials.org.au/ (accessed 16 July 2025).
35 WA Consumer and Community Involvement Program. cciprogram.org/ (accessed 9 July 2025)
36 National Centre for Indigenous Genomics (NCIG). ncig.anu.edu.au/ (accessed 9 July 2025)
37 National Rural Health Alliance 2024–25 Pre-Budget Submission (2024). www.ruralhealth.org.au/wp-content/uploads/2024/11/national-rural-health-alliance-pre-budget-submission-2024-25.pdf. (accessed 17 July 2025)
38 Alston L and Versace VL (2023). Place-based research in small rural hospitals: an overlooked opportunity for action to reduce health inequities in Australia? The Lancet Regional Health – Western Pacific, Vol 30, No. 100682. www.thelancet.com/journals/lanwpc/article/PIIS2666-6065(22)00297-8/fulltext
39 Barclay L, Phillips A and Lyle D (2018). Rural and remote health research: Does the investment match the need? Aust. J. Rural Health, Vol 26, pp 74–79. onlinelibrary.wiley.com/doi/full/10.1111/ajr.12429 (accessed 16 July 2025)
40 Moran A, Haines H, Raschke N, Schmidt D, Koschel A, Stephens A, Opie C, Nancarrow S (2019). Mind the gap: is it time to invest in embedded researchers in regional, rural and remote health services to address health outcome discrepancies for those living in rural, remote and regional areas? Australian Journal of Primary Health 25, 104-107. www.publish.csiro.au/py/PY18201
41 O’Sullivan B, Cairns A and Gurney T (2020). Exploring how to sustain ‘place-based’ rural health academic research for informing rural health systems: a qualitative investigation. Health Res Policy Sys, Vol 18, No. 90. doi.org/10.1186/s12961-020-00608-7
42 Wong A, Quilliam C, Corboy D et al (2022). What shapes research and research capacity building in rural health services? Context matters. Aust J Rural Health, Vol 30, pp 410-421. https://doi.org/10.1111/ajr.12852
43 Townsville Institute of Health Research and Innovation. www.townsville.health.qld.gov.au/research/for-researchers/townsville-institute-of-health-research-and-innovation/ (accessed 16 July 2025)
44 Aboriginal Health & Medical Research Council of NSW. Policy Priorities 2021. www.ahmrc.org.au/wp-content/uploads/2023/10/AHM_Policy-Priorities-document-2021_Online.pdf (accessed 16 July 2025)
45 NHMRC. Annual Report 2023–24, Canberra: National Health and Medical Research Council, 2024. www.nhmrc.gov.au/about-us/corporate-plans-and-annual-reports (accessed 8 July 2025)
46 Medical Research Future Fund. Indigenous Health Research Fund Roadmap. www.health.gov.au/sites/default/files/2023-11/mrff-indigenous-health-research-fund-strategic-documents.pdf (accessed 8 July 2025)
47 Productivity Commission (2024). Closing the Gap Annual Data Compilation Report July 2024, Canberra. pc.gov.au/closing-the-gap-data/annual-data-report/closing-the-gap-annual-data-compilation-july2024.pdf (accessed 16 July 2025)
48 Department of Health, Disability and Ageing (2024). Medical Research Future Fund Report on Chief Investigator data. www.health.gov.au/resources/publications/medical-research-future-fund-report-on-chief-investigator-data?language=en (accessed 8 July 2025)
49 National Aboriginal Community Controlled Health Organisation (NACCHO) (2011). Constitution for the National Aboriginal Community Controlled Health Organisation. f.hubspotusercontent10.net/hubfs/5328468/NACCHO_April_2020/PDFs/NACCHO-CONSTITUTION-Ratified-Ver-151111-for-ASIC-.pdf (accessed 16 July 2025).
50 Jones R, Thurber KA, Chapman J, et al (2018). Study protocol: Our Cultures Count, the Mayi Kuwayu Study, a national longitudinal study of Aboriginal and Torres Strait Islander wellbeing. BMJ Open, Vol 8, e023861. http://doi: 10.1136/bmjopen-2018-023861.
51 Maiam nayri Wingara (2018). Indigenous Data Sovereignty Communique Indigenous Data Sovereignty Summit 20th June 2018. Canberra, Australia. Available from: www.maiamnayriwingara.org/mnw-principles (accessed 22 July 2025)
52 NHMRC Targeted Calls for Research. www.nhmrc.gov.au/research-policy/research-priorities/guide-proposing-targeted-calls-research (accessed 9 July 2025)
53 NHMRC. National Health and Medical Research Council Road Map 3: A strategic framework for improving Aboriginal and Torres Strait Islander health through research. Report of Community Consultations. www.nhmrc.gov.au/health-advice/aboriginal-and-torres-strait-islander-health/road-map-3 (accessed 16 July 2025)
54 McKenzie C, Bandler LG (2023). Aboriginal and Torres Strait Islander health research leadership. Med J Aust. Vol 218, No. 2, pp 75-6.
55 Laird P, Chang AB, Jacky J et al (2021). Conducting decolonizing research and practice with Australian First Nations to close the health gap. Health Res Policy Sys, Vol 19, No 127.
56 Thurber KA, Thandrayen J, Banks E, Doery K, Sedgwick M, Lovett R (2020). Strengths-based approaches for quantitative data analysis: A case study using the Australian Longitudinal Study of Indigenous Children. SSM Popul Health Vol 6, No. 12:100637. doi: 10.1016/j.ssmph.2020.100637.
57 McGuffog R, Bryant J, Booth K, Collis F, Brown A, Hughes JT, Chamberlain C, McGhie A, Hobden B, Kennedy M (2023). Exploring the Reported Strengths and Limitations of Aboriginal and Torres Strait Islander Health Research: A Narrative Review of Intervention Studies. Int J Environ Res Public Health, Vol 20, No. 5, pp 3993.
58 Lowitja Institute – Research Grants. www.lowitja.org.au/research/research-grants/ (accessed 8 July 2025)
59 Network Environments for Indigenous Health Research (NEIHR). cihr-irsc.gc.ca/e/51161.html (accessed 21 August 2025)
60 NHMRC. Fact sheet: Benefit for Aboriginal and/or Torres Strait Islander health question – Centres of Research Excellence 2025 pilot. www.nhmrc.gov.au/about-us/resources/fact-sheet-benefit-aboriginal-torres-strait-islander-health-question-cre-pilot (accessed 9 July 2025)
61 Kimberley Aboriginal Health Research Alliance. www.kahra.org.au/principles (accessed 8 July 2025)
62 Central Australian Academic Health Science Network. caahsn.org.au/our-story-so-far/ (accessed 8 July 2025)
63 Our Collaborations in health research (OCHRe). public-health.uq.edu.au/project/ochre-our-collaborations-health-research (accessed 9 July 2025)
64 Zurynski Y, Smith CL, Vedovi A, Ellis LA, Knaggs G, Meulenbroeks I, Warwick M, Gul H, Pomare C, Braithwaite J (2020). Mapping the Learning Health System: A Scoping Review of Current Evidence. Australian Institute of Health Innovation, and the NHRMC Partnership Centre for Health System Sustainability.Sydney, Australia. www.mq.edu.au/__data/assets/pdf_file/0011/1083809/Mapping-the-Learning-Health-System-A-white-paper-web.pdf (accessed 16 July 2025)
65 Symons T, Woollett A, Zalcberg J, Eckstein L (2024). Implementing Decentralized Clinical Trials in Australia through Teletrials: Where to From Here? Therapeutic Innovation & Regulatory Science australianteletrialprogram.gov.au/wp-content/uploads/2024/08/DIA-Teletrials-Paper-Apr-24.pdf (accessed 17 July 2025).
66 The Australian Health Research Alliance. ahra.org.au/ (accessed 9 July 2025)
67 AusBiotech submission in response to the Industry Growth Program: Consultation Paper. www.ausbiotech.org/documents/item/772 (accessed 16 July 2025)
68 Australian Government Department of Industry, Science and Resources. Domestic business environment. www.industry.gov.au/publications/australian-innovation-statistics/domestic-business-environment (accessed 16 July 2025)
69 MTPConnect (2021). MTPConnect REDI Initiative Skills Gap Analysis Second Report. www.mtpconnect.org.au/images/MTPC%20REDI%20Skills%20Gap%20Second%20Report.pdf (accessed 17 July 2025)
70 MTPConnect – Australia’s Life Sciences Innovation Accelerator. www.mtpconnect.org.au/ (accessed 16 July 2025)
71 The European Innovation Council. eic.ec.europa.eu/index_en (accessed 16 July 2025)
72 Australian Government Department of Industry, Science and Resources (2024). Medical Science Co-investment Plan. www.industry.gov.au/sites/default/files/2024-04/medical_science_co-investment_plan.pdf (accessed 16 July 2025)
73 Ausbiotech. Biotechnology Blueprint - A Decadal Strategy for the Australian Biotechnology Industry. www.ausbiotech.org/documents/item/703 (accessed 16 July 2025)
74 AusBiotech and MTPConnect (2024). National Biotech and Medtech Development and Commercialisation Summit 2024 Discussion Paper. www.mtpconnect.org.au/images/AusBiotech_MTPConnect_DiscussionPaper2024.pdf (accessed 16 July 2025)
75 NSW Innovation and Productivity Council (2018). NSW Innovation Precincts Lessons from international experience. www.investment.nsw.gov.au/assets/Uploads/files/IPC/Full-Report-IPC-NSW-Innovation-Precincts-2018.pdf (accessed 16 July 2025)
76 Anteris Technologies. anteristech.com/about-us.html (accessed 16 July 2025)
77 Markets and Markets (2025). Artificial Intelligence in Healthcare Market. www.marketsandmarkets.com/Market-Reports/artificial-intelligence-healthcare-market-54679303.html
78 Australian Digital Health Agency (2023). National Digital Health Strategy 2023-2028. www.digitalhealth.gov.au/sites/default/files/documents/national-digital-health-strategy-2023-2028.pdf (accessed 16 July 2025)
79 The Centre for Health Record Linkage (CHeReL). www.cherel.org.au/about-us (accessed 16 July 2025).
80 Singapore Integrated Diabetic Retinopathy Programme (SiDRP). www.snec.com.sg/our-specialties/clinic-locations/sidrp (accessed 16 July 2025)
81 World Health Organisation (2023). Climate Change. WHO Factsheet. www.who.int/news-room/fact-sheets/detail/climate-change-and-health (accessed 21 August 2025)
82 Australian Department of Health, Disability and Ageing. National Health and Climate Strategy (2023). www.health.gov.au/sites/default/files/2023-12/national-health-and-climate-strategy.pdf (accessed 16 July 2025)
83 Tasmanian Government. Climate Change (State Action) Act 2008. (Tas) s5., 2022. www.legislation.tas.gov.au/view/pdf/authorised/2022-11-30%202022-12-13/act-2008-036 (accessed 16 July 2025)
84 Tasmanian Health Department (2019). Tasmanian climate change and health roundtable – Final Report. Tasmanian Government. www.health.tas.gov.au/publications/tasmanian-climate-change-and-health-roundtable-report (accessed 21 August 2025)
85 Australian Commission on Safety and Quality in Health Care (2024). Joint Statement: Working together to achieve sustainable high-quality health care in a changing climate. www.safetyandquality.gov.au/publications-and-resources/resource-library/joint-statement-working-together-achieve-sustainable-high-quality-health-care-changing-climate (accessed 16 July 2025).
86 National Institute for Health and Care Research (NIHR) Our commitments to climate, health and sustainability 2024-2026. www.nihr.ac.uk/our-commitments-climate-health-and-sustainability-2024-2026 (accessed 16 July 2025).
87 Wellcome Trust. Concordat for the Environmental Sustainability of Research and Innovation Practice. wellcome.org/about-us/positions-and-statements/environmental-sustainability-concordat (accessed 16 July 2025).
88 Australian Government Department of Health, Disability and Ageing (2024) The Australian Health and Medical Research Workforce Audit – October 2024. www.health.gov.au/resources/publications/mrff-the-australian-health-and-medical-research-workforce-audit?language=en (accessed 16 July 2025).
89 Aksnes DW, Sivertsen G (2023) Global trends in international research collaboration, 1980-2021①[J]. Journal of Data and Information Science, Vol 8, No. 2, pp 26-42 doi.org/10.2478/jdis-2023-0015.
90 Australian Government Indo-Pacific Centre for Health Security. Investments. indopacifichealthsecurity.dfat.gov.au/investments (accessed 16 July 2025).
91 World Health Organization (2023) Investing in cervical cancer elimination across Australia and the Indo–Pacific, 17 November 2023. www.who.int/news/item/17-11-2023-investing-in-cervical-cancer-elimination-across-australia-and-the-indo-pacific (accessed 16 July 2025).
92 The Daffodil Centre (2023) Australia takes ‘EPICC’ step towards fairer cervical cancer outcomes in region. daffodilcentre.org/australia-takes-epicc-step-towards-fairer-cervical-cancer-outcomes-in-region/ (accessed 16 July 2025).