The Melbourne Academic Centre for Health is an NHMRC-accredited Research Translation Centre. We collaborate to deliver research-informed healthcare and training. The below case studies highlight our work in translating research into better health outcomes and building capability across the system.
Case studies on this page:
- Developing, re-designing or adopting platforms, systems or workforce initiatives: Clinical trials workforce development through A-CTEC.
- Providing better care: The MacHSR future leaders fellowship program
- Meeting the needs of your end-users in your population: Developing research-led nurse and AHP innovators in advanced practice

Case studies from all Research Translation Centres are available from Impact and outcomes.
Developing, re-designing or adopting platforms, systems or workforce initiatives: Clinical trials workforce development through A-CTEC
Challenge
Clinical trials are an essential part of healthcare improvement. The National Clinical Trials Governance Framework (NCTGF) is now being implemented nationwide by the Australian Commission on Safety and Quality in Healthcare (ACSQH) as part of the Commission’s periodic mandatory accreditation of Health Services. Success in the latter requires ACSQH to approve adherence to the NCTGF, which includes a requirement that all Health Service staff involved in trials have been trained to an appropriate level.
Approach
To meet the NCTGF-imposed need for training in clinical trials, easily accessible in settings from remote to metropolitan, the precursor of what is now the online, free at the point of use platform the Australian Clinical Trials Education Centre (A-CTEC) was originally developed by the Melbourne Academic Centre for Health (MACH) partners for local use.
Rapid dissemination across Victoria of the positively evaluated MACH platform was achieved in 2022 with the launch of the Victorian Clinical Trials Education Centre (V-CTEC) – a collaboration of the 3 Victorian Research Translation Centres: MACH, Monash Partners Academic Health Science Centre and Western Alliance – following extensive consultation and codesign with key stakeholders.
At the request of various state governments and with support from ACSQH, V-CTEC was scaled nationally and rebranded as A-CTEC in 2023, providing interactive, practical, multi-modal and evidence-based education modules and training through its open access platform for the clinical trials workforce across Australia at no charge to the end user.
The platform is financed through state and territory-based subscriptions totalling $380,000 per annum to enable access for users within each jurisdiction.
National governance of A-CTEC continues to be overseen by MACH in collaboration with Monash Partners and Western Alliance and is administered by Cancer Trials Australia, to maintain stakeholder relationships and ensure the platform meets the needs of the end users and each state and territory.
Significance
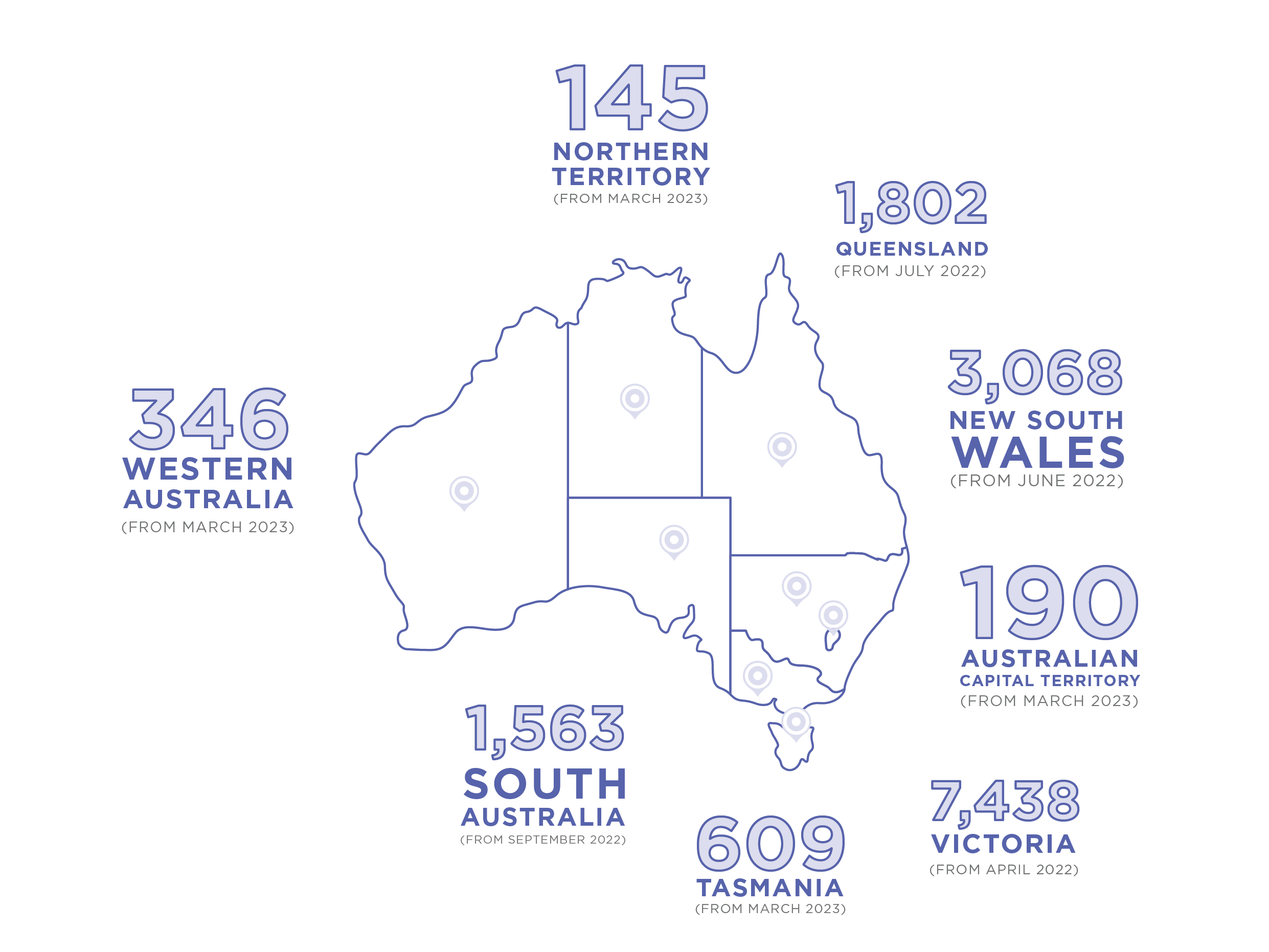
Currently all jurisdictions across Australia subscribe to A-CTEC with, as of July 2025, 15,129 registered users nationally.
A-CTEC builds the capacity and capability of the clinical trials workforce in Australia by delivering standardised education and training that is internationally recognised and in doing so supports health services to comply with the NCTGF.
The partnership with A-CTEC was recently highlighted as a key priority of the Victorian Government providing training and upskilling programs which address skill gaps in clinical trials (see: Victoria’s Health and Medical Research Workforce Action Plan December 2024).
A-CTEC significantly reduces the training delivery and administrative burden on individual organisations delivering and overseeing clinical trials compliance across their institution, resulting in time and budget savings across each state and territory.
Value-add of centre
A-CTEC would not have come into being without the initial collaborations within MACH and leadership by MACH across Victoria then Australia.
Reach
As of July 2025, registered users were:
Next steps
Achieving financial sustainability of the platform, independent of governments, without an administrative burden to Health Services or cost to end users, is now a top priority. A solution may lie in growing interest from international jurisdictions prepared to pay to allow their staff to access A-CTEC.
Providing better care: The MacHSR future leaders fellowship program
Challenge
Health systems are grappling with major shared problems such as unsustainable pressure on hospital services, inequitable access to evidence-based care, and low value care. Furthermore, every Health Service has specific problems obvious to consumers and frontline clinicians and identified as priority problems by the organisational leadership.
Across the Melbourne Academic Centre for Health (MACH) partner health services, frontline clinicians with little Health Services Research (HSR) expertise are keen to learn how to fix the prioritised problems in front of them by co-designing, evidencing, implementing and evaluating HSR-based solutions such as new models of care.
Approach
Reasoning that clinical leadership is a powerful means of driving adoption of evidence-based better care, in 2022, MACH established the $500,000 per annum self-funded MacHSR Future Leaders Fellowship Program to upskill clinicians in HSR, providing them with the skills to address issues in their health services and share their knowledge across their organisations, whilst remaining at the clinical frontline.
Each year, MACH seeks to competitively recruit a clinician from every MACH health service plus one from primary care, to solve practical care-delivery problems that have been identified by their health services in discussion with local consumers as an executive level priority. Each Health Service ranks its applicants’ proposed projects for relevance to local priorities.
Appointed MacHSR Fellows are funded by their health service (cash total $50,000 per annum) to complete in their own time over 6 months the Introduction to HSR elective in the University of Melbourne’s Master of Public Health program, to ensure high quality training in HSR methodologies.
Then, for one year each Fellow receives 0.2 Full-Time Equivalent (FTE) protected research and translation time (in kind from Health Services totalling $350,000 per annum) and expert academic supervision (in kind from UoM totalling $100,000 per annum).
A key objective of the program is to bring collaborative health service-led research pilots to a stage where follow-on research and translation funding can be built around a MacHSR 'Graduate' and the supervisory health service researchers.
Significance
To date, 39 clinicians from a wide range of disciplines have completed (cohorts 1&2) or are undertaking (cohorts 3&4) a MacHSR Fellowship. View a full list of projects.
Examples of better care already delivered by MacHSR Fellows and their supporters include:
- Successful implementation of same day surgery for certain procedures, reducing the number of overnight stays and associated costs at the Royal Melbourne Hospital (RMH), without an increase in readmissions
- A newly-evidenced and implemented diagnostic protocol at St Vincent’s Hospital Melbourne (SVHM) defining artefactual blood troponin elevation in patients with suspected acute coronary syndrome has reduced unnecessary investigations and admissions for those without myocardial injury
- Implementation and evaluation at Royal Children’s Hospital (RCH) of remote symptom monitoring and automated treatment plans for children with cystic fibrosis have identified exacerbations requiring rapid treatment without increased hospital visits.
Value-add of centre
Providing better care through MacHSR requires (future) clinical leaders to collaborate across centre partners with HSR experts relevant to the priority. On one hand such collaboration upskills MacHSR Fellows, while on the other it draws HSR experts into addressing problems prioritised by MACH’s end-users – this would not happen without MACH.
Reach
Projects undertaken by the MacHSR Fellows have addressed a broad selection of health service delivery issues across MACH partners. Fellows have shared their knowledge, upskilling colleagues at the clinical frontline in other Health Services and engaging Victorian Government with the demonstrated solutions (for example, day surgery).
Next steps
MACH’s desire to accelerate follow-on delivery of strategically important MacHSR Fellowship programs is our priority for use of the recently awarded NHMRC RTC Support funding.
Despite much effort and various incentives, we have so far failed to attract applications from potential Aboriginal MacHSR Fellows (possibly in keeping with so few MACH-affiliated clinicians being Aboriginal), but we hope that our recent engagement with the Melbourne Poche Centre Indigenous Health Leadership program will, in time, lead to Aboriginal applicants coming forward.
Meeting the needs of your end-users in your population: Developing research-led nurse and AHP innovators in advanced practice
Challenge
The Melbourne Academic Centre for Health (MACH)-affiliated Health Service CEOs are key end-users of research. They are keen to develop a cadre of PhD-trained nurses and AHPs (Allied Health Professionals) capable of leading the innovation and implementation of new models of care that are led and delivered by nurses and AHPs practicing in advanced care roles. This will bypass unnecessary dependence of care pathways on limited doctor availability, improve consumer access and decrease cost.
However, across MACH there had been no systematic approach to develop the research-led nurse and AHP innovators needed by combining clinical training for advanced practice roles with research training to PhD and beyond; the opportunities had been 'either/or'.
Approach
At reaccreditation in 2022, in response to expressions of need from end-user Health Service CEOs, MACH committed to expand the successful self-funded 5-year MACH-Track program from medics in specialist vocational training only to include nurses, midwives and physiotherapists (NMPs) in the first instance.
This came with a requirement to combine research training in developing new NMP-led models of care with clinical training to advanced practice level, placing additional financial (approximately $1 million per annum) and organisational demands on all MACH partners.
MACH-Track seeks to develop with intensive support only a small number of trainees with outstanding leadership potential – 5 medics and 3 NMPs each year since 2022.
Nevertheless the expansion required University of Melbourne (UoM) to increase the annual allocation to MACH-Track of prestigious 3-year Research Training Program PhD scholarships from 5 to 8 (steady state UoM cash contribution increasing from 15 × ~$38,000 = ~$570,000 per annum to 24 × ~$38,000 = ~$912,000 per annum) with a commensurate increase in cash contributions from the research partner hosting the PhD, UoM or Medical Research Institutes, for the 75% PhD stipend 'top-up' intended to minimise earnings loss (at steady state increasing from 15 × ~$29,000 = $435,000 per annum to 24 × ~$29,000 = ~$696,000 per annum).
Furthermore, Health Services needed to increase the steady state in-kind contribution of allowing MACH-Track trainees 0.2 Full Time Equivalent (FTE) research release in the pre-PhD and post-PhD years by 6 × ~$30,000 = ~$180,000 per annum, and to increase the steady state cash contribution to provide a paid supernumerary 0.2FTE clinical training post during the three PhD years, rising by 9 × ~$30,000 = ~$270,000 per annum.
Furthermore, each Health Service with a NMP 'on track' needed to organise for a given trainee, at unquantifiable cost, a bespoke 5-year clinical practice development program to reach advanced practice level (for example, Nurse Practitioner or Grade 4 Specialist Physiotherapist).
Significance
By allowing outstanding NMPs access to the medical pool on merit, following the 2022, 2023 and 2024 recruitment processes we now have 11 NMPs (rather than the anticipated 9) 'on track', 6 nurses, 4 physios and 1 midwife, roughly in proportion to the head counts in these disciplines across our Health Services, with appropriate diversity including gender balance (10 female and 1 male).
All are working on co-design, evidencing and implementing new NMP-led models of care through their PhD studies, whilst being supported to develop their own progression to competency for advanced practice (which helpfully is determined by their parent Health Service, rather than by Royal and Specialist Colleges, as for the medics).
Value-add of centre
Without MACH and its collaborative ethos, MACH-Track as a means to combine research and clinical training for future leader development would not have come into being. Without responsiveness to end-user need, and commitment to the financial and organisational burden on MACH partners necessary to respond, expansion to NMPs could not have occurred.
Reach
New NMP-led models of care and the innovators required to lead them are now in development in 11 important domains for end-users - in prehabilitation to diminish complications of elective surgery; care of chronic spinal cord injury; respite care of children with severe neurological impairment; care co-ordination for Intensive Care Unit survivors; abortion care; post-surgical care for endometrial cancer survivors; embedding NMP-led clinical trials in the electronic medical record; reducing Emergency Department waiting times; NMP-led improvements in the living kidney donation care pathway; and incorporating patient-related outcomes into prioritisation of patients wait-listed for orthopaedic surgery.
Already, 6 of 10 MACH-affiliated Health Services have at least one NMP 'on track'.
Next steps
Three priorities are:
- Encourage our first Aboriginal NMP applicant to MACH-Track, which we hope to do (through engagement with the Melbourne Poche Centre’s Indigenous Health Leadership Program)
- Expand further to a total of 10 appointments per year to allow access for all AHP disciplines and dentistry
- Confirm our prediction that appointment on merit alone will place non-medical MACH-Trackers across all 10 Health Service partners.

