Microsurgery describes surgical procedures performed using a microscope and specialised tools. It is often used to connect small structures in the body such as blood vessels, nerves and lymphatics. NHMRC-funded researchers in (what is now) the O’Brien Department of St Vincent’s Institute of Medical Research have been at the forefront of developing microsurgery since its emergence during the mid-20th century. Their pioneering precision instruments, microsurgical techniques and research models revolutionised surgical practice, allowing countless patients worldwide to receive a standard of surgical reconstruction for their injuries that was previously impossible.
Origin
Plastic and reconstructive surgery is a surgical speciality that aims to restore or improve the form and function of body parts affected by illness, trauma or congenital disease. In the absence of the ability to close a wound directly, or to use a skin graft, a flap must be used. A skin graft is a shaving of tissue that is totally separated from the body. Because it is thin it can restore blood flow by growth of blood vessels from the graft. A flap by contrast, is a composite unit of tissue, usually skin and fat and is too thick to restore blood flow spontaneously. It requires connection to an intact blood supply throughout the transfer process to stay ‘alive’. Flaps are the mainstay of plastic surgical reconstruction and come in several different shapes and forms. They are classified according to their source and how they are transferred.
For much of the 1900s, pedicled flaps were the standard approach for reconstructing major injuries to upper or lower limbs. For the mobilised donor flap to reach the target site and still retain a critical vascular attachment at its base (pedicle), it had to be designed immediately adjacent to the defect. This requirement limited the flap’s application. To transfer a flap from a distance was a complex and unreliable process requiring multiple staged transfers taking several months.
The solution did not arrive until it was realised that some tissues in the body survived on single small blood vessels and that theoretically, by joining these vessels to equivalent ones at the recipient site, the tissue flap could be transferred in one operation. This was to become known as a microvascular free tissue transfer or ‘free flap’. However, the small size of the involved blood vessels proved a serious technical challenge.
In the mid-1960s, Bernard O’Brien, an assistant plastic surgeon at St. Vincent’s Hospital, Melbourne, began his studies on the re-connection of small blood vessels and repair of severed nerves. During his training in New York, he became aware of the earliest attempts at small vessel repair facilitated by advances in microscope design and visited several centres including in San Francisco and Moscow, where lymphatic surgery was being attempted. He saw the clinical potential that success in this field could bring.
Investment
O’Brien established the Microsurgery Research Centre, as it was initially called, as a privately funded independent entity in the grounds of St Vincent’s hospital and pursued targeted research into microvascular surgery. From 1969, the Centre was supported by numerous NHMRC Project grants. In 1972, O’Brien established an international fellowship for training and research in microsurgery at St Vincent’s, supported by funding from NHMRC. This core funding facilitated philanthropic funding and the establishment of (what is now) the O’Brien Foundation. The Centre also received funding from the Victorian State Government and the Brockhoff Foundation.
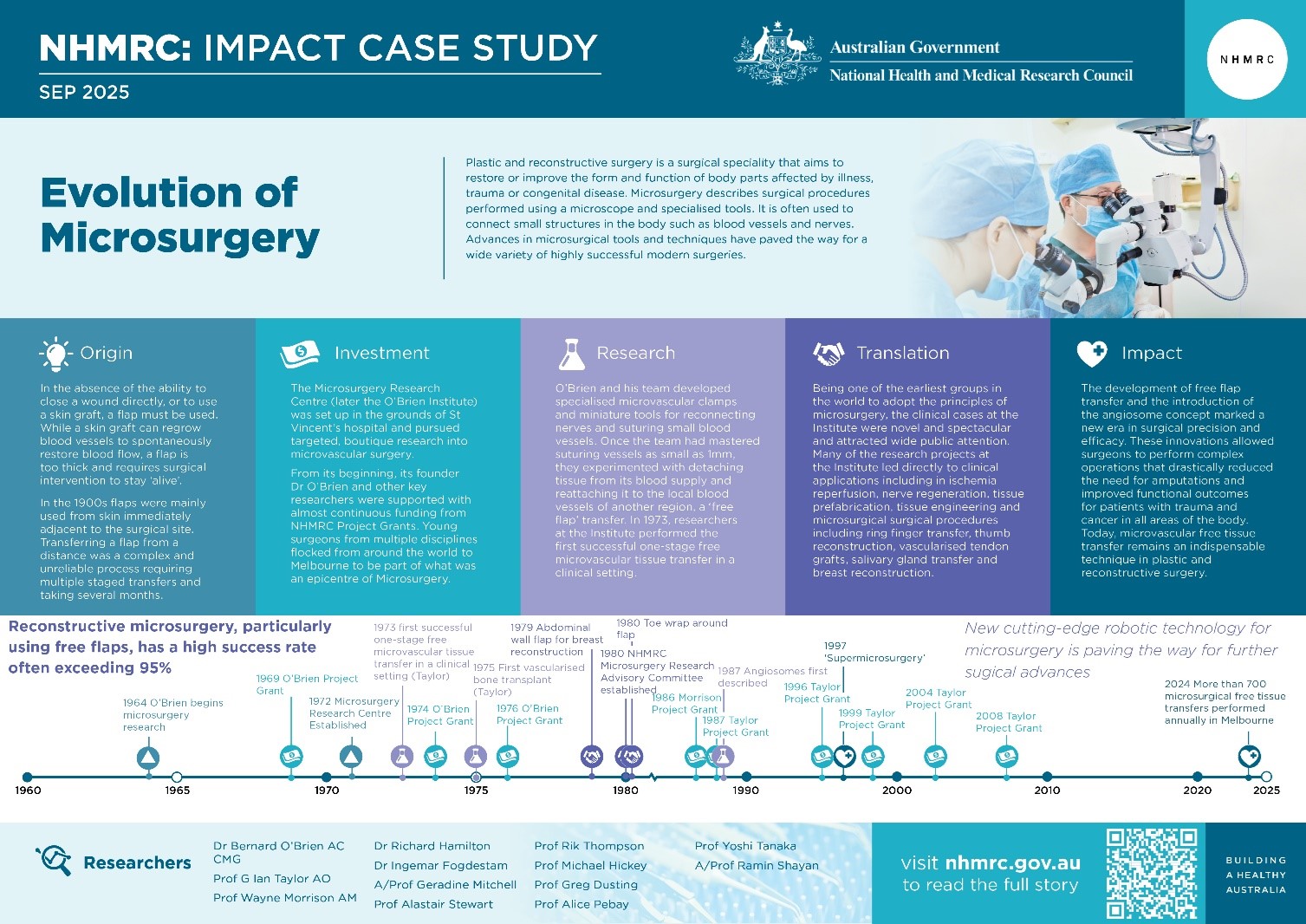
The PDF poster version of this case study includes a graphical timeline showing NHMRC grants provided and other events described in the case study.
Research
From 1969 to 1972, O’Brien and his team conducted a series of trials on small artery and nerve repairs. Operating on these tiny structures required the use of specialised instruments which had to be created by O’Brien’s team. The team modified microscopes, and with the help of Professor Gerard Crock in the Department of Ophthalmology and local instrument makers, developed specialised microvascular clamps and crafted miniature tools for reconnecting nerves and suturing small blood vessels.1,2,3,4 Once the team had mastered suturing vessels as small as 1mm, they experimented with detaching tissue from its blood supply and reattaching it to the local blood vessels of another region, known as a free flap transfer. 5,6,7,8 He and his team applied the techniques clinically for replantation of amputated parts particularly digits and limbs, a field not previously possible.

In 1973, plastic surgeon Ian Taylor encountered a patient with severe skin loss over an exposed ankle joint— a condition that, in the past, would have required amputation as the only viable treatment.9 Taylor asked Rollin Daniel, an international research fellow from the O’Brien Institute, to assist him to perform the free flap microsurgery on the patient.10 The microsurgery was a success, representing the first clinically successful one-stage free microvascular tissue transfer.11 Later in the same year O’Brien and his team performed the second successful transfer for a gunshot wound in the foot.12
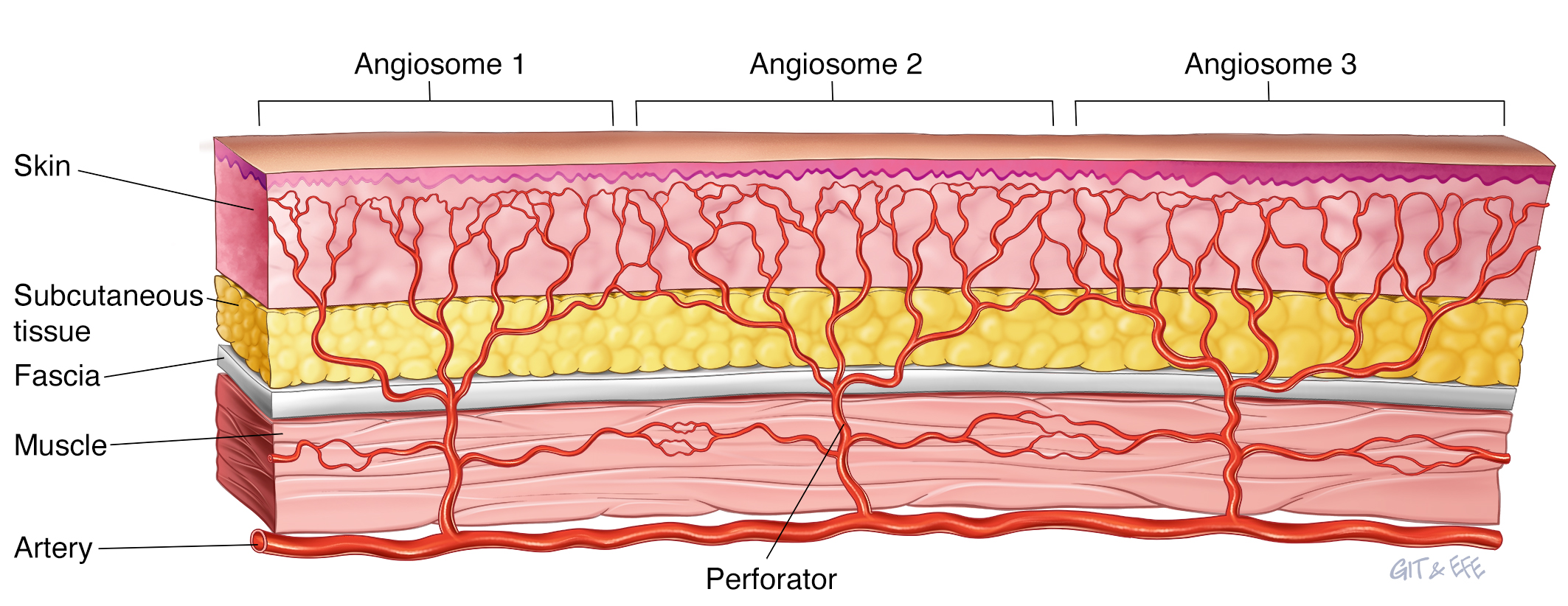
Taylor subsequently established his own research team, the Jack Brockhoff Reconstructive Plastic Surgery Research Unit, affiliated with the Anatomy Department at University of Melbourne. Supported by NHMRC, this team investigated the detailed vascular anatomy of the body. This led to his widely acclaimed angiosome concept of blood supply, where a 3-dimensional block of tissue including, skin, muscle and bone, is supplied by an artery and drained by a vein. While the idea of blood vessels called ‘perforators’ feeding tissue from a deeper source had been described before, Taylor’s detailed and meticulous mapping was a milestone in the clinical advancement of microsurgery.13 It allowed for a greater understanding of the nuances of flap survival, defining the blood supply to new and expendable donor sites for free vascularised tissue transfer containing various combinations of skin, muscle, tendon and bone14,15,16,17 and helped in the refinement of new surgeries.18 These include the first successful free vascularised transfer of living bone (1975; nerve (1976) and tendon (1979).
Translation
Being one of the first groups in the world to adopt the principles of microsurgery, the clinical cases at the O’Brien Institute were novel and attracted wide public attention. The large volume of cases built a substantial collection of clinical experiences, resulting in numerous national and international presentations, scientific publications, books and book chapters. This in turn attracted students and clinicians from around the world, with more than 200 international fellows trained at the O’Brien Institute and many on their return, becoming leaders in their field.
A key area benefiting from this research was breast reconstruction. Mastectomy was a frequent outcome in the treatment (and later prevention) of breast cancer, yet reconstructive options for post-mastectomy patients were limited.19 In 1978, Ingemar Fogdestam and Richard Hamilton, while fellows at the O’Brien Institute, carried out multiple studies to define the vascular anatomy of the abdominal wall and its potential use as a free flap transfer for breast reconstruction.20,21 This surgery has become the ‘gold standard’ operation for breast reconstruction, and one of the most commonly performed procedures in the repertoire of microsurgery.
Another revelation, pioneered by Taylor, has been the introduction of vascularised bone to reconstruct the jaw following trauma or major cancer surgery using the fibula16 from the leg or the iliac bone from the hip.17 The type of injury often suffered in World War I and World War II which took months or years to repair, can now be accomplished in a matter of hours.
Several original microsurgical procedures have been developed and published by the research team, all stemming from the foundational microsurgical research studies. Some of these include:
- Thumb reconstruction using a wrap-around flap. This technique is now considered best practice for thumb reconstruction22,23
- Ring finger transfer which enables the restoration of gripping function to a mutilated hand
- The scapular flap which uses tissue from the scapula and can provide a large area of tissue for transfer
- Vascularised tendon grafts; transplanting tendons while maintaining blood supply
- Salivary gland transfer for treatment of persistent dry eye disease (intractable Xerophthalmia)
- Micro-sympathectomy (a microsurgical technique to remove nerve fibres to manage pain and improve blood flow) for treatment of scleroderma
- Lymphoedema treatment by multiple microsurgical techniques to address the swelling of tissues due to build up of lymph fluid.
Outcomes and impacts
The development of free microvascular (free flap) transfer and the introduction of the angiosome concept marked a new era in surgical precision and efficacy. These innovations allowed surgeons to perform complex operations that drastically reduced the need for amputations and improved functional outcomes for patients with trauma and cancer in all areas of the body.24
Today, microvascular free tissue transfer remains an indispensable technique in plastic and reconstructive surgery, serving as the benchmark for reconstructing significant soft tissue and bony defects following cancer resection and trauma. It is used across various specialties, including general surgery, ophthalmology, orthopaedic surgery, neurosurgery and paediatric surgery. Common procedures using this technique include toe and digit replantation, lymphatic reconstruction for lymphoedema, complex wound reconstruction, head and neck reconstruction, and breast reconstruction. In Melbourne and surrounds alone, more than 700 microsurgical free tissue transfers are performed each year.
Advancements in breast reconstruction, redefined options for post-mastectomy patients by offering better aesthetic and functional results while minimising donor site complications. Breast cancer is the most commonly diagnosed cancer for females in Australia25, and approximately 40% of women diagnosed with breast cancer undergo a mastectomy.26 Studies have shown that breast reconstruction can have positive benefits on patients’ psychological health, including their body image and emotional and social well-being. Offering breast reconstruction at the time of mastectomy is now a standard of care in Australia.27
Researchers
Dr Bernard O’Brien AC CMG
Bernard McCarthy O’Brien studied science and medicine at the University of Melbourne (UoM), graduating in 1950. He undertook his residency at St Vincent's Hospital in Melbourne before working as a demonstrator and clinical assistant at UoM (1953-1954). After obtaining his Master of Surgery degree in 1955, O’Brien pursued further surgical training in England and New York. On his return to Melbourne, he established the Microsurgery Research Centre (subsequently the O’Brien Institute) in 1972 and served as its director until 1992. O’Brien obtained his Doctor of Medicine in 1978 from UoM and in 1992 was awarded the Sir Hugh Devine Medal, the highest honour from the Royal Australasian College of Surgeons. He was appointed Companion of the Order of St Michael and St George in 1982 and Companion of the Order of Australia 1991.
Professor Geoffrey Ian Taylor AO
Geoffrey Ian Taylor received his undergraduate medicine degree from The University of Melbourne in 1963 before obtaining his Doctor of Medicine in 1991. He joined the Royal Melbourne Hospital (RMH) as an Honorary Assistant Plastic Surgeon in 1969 and was awarded the prestigious Hunterian Professorship by the Royal College of Surgeons of England for 1981. Taylor became the Head of RMH’s Plastic and Reconstructive Surgery Unit from 1992–2002 and is currently Head of the Jack Brockhoff Reconstructive Plastic Surgery Research Unit at the University of Melbourne. Taylor was appointed an Officer of the Order of Australia in 1999, awarded the Excellence in Surgery award from the Royal Australasian College of Surgeons in 2006 and inducted into the Royal Melbourne Hospitals Hall of Fame in 2016.
Professor Wayne Morrison AM
Wayne Morrison undertook his medical studies at UoM, graduating in 1967. He trained in plastic and hand surgery at St Vincent's Hospital, Melbourne and underwent further training overseas in the United Kingdom, France, and the United States. He became a Professor of Surgery at UoM department surgery and Head of St Vincent’s Plastic Surgery Unit in 1991, and the Director of the O'Brien Institute in 1992. He was president of the World Society of Microsurgery, the Asian Pacific Federation of Societies for surgery of the Hand and the Australian Hand Surgery Society. Awarded the Australian and New Zealand Head and Neck Cancer Society Medal of Excellence in 2013 and was nominated a Pioneer of Hand Surgery by the International Federation of Societies for Surgery of the Hand in 2016. He was appointed a Member of the Order of Australia in 2001.
Dr Richard Hamilton
Richard Hamilton graduated from medicine at the University of Adelaide Medical School in 1970 and undertook surgical training for the next decade in Melbourne, Adelaide, Sweden, and New Zealand. He was the Head of Plastic Surgery at Flinders Medical Centre from 1980 to 1995 and established its microsurgical service. Hamilton is currently the Chief Plastic Surgeon at Hamilton House Plastic Surgery in Adelaide.
Dr Ingemar Fogdestam
Ingemar Fogdestam completed his medical degree in Sweden and undertook a fellowship at the Microsurgery Research Centre in St Vincent’s Hospital from 1977–1978. After his fellowship, he returned to Sahlgrenska University Hospital in Sweden and established Sweden’s first microsurgical service. Prior to retiring, he was an Associate Professor of Plastic Surgery at the Sahlgrenska Academy of Göteborg University.
Other Researchers
Other researchers that contributed to the impacts described in this case study include Associate Professor Geraldine Mitchell, Professor Alastair Stewart, Professor Rik Thompson, Professor Michael Hickey, Professor Greg Dusting, Professor Alice Pebay, Professor Yoshi Tanaka and Associate Professor Ramin Shayan.
Partner
This case study was developed in partnership with St. Vincent’s Institute of Medical Research.

References
The information and images from which impact case studies are produced may be obtained from a number of sources including our case study partner, NHMRC’s internal records and publicly available materials. Key sources of information consulted for this case study include:
Books
Microvascular Reconstructive Surgery Churchill Livingstone 1977
Reconstructive Microsurgery; O’Brien and Morrison, Churchill Livingstone 1986
The Angiosome Concept and Tissue Transfer. Taylor GI, Pan WR. Assoc Ed Dodwell P, Pub CRC Press, ISBN 9781576261613, Nov 2013.
Publications
1O'Brien B. The Triploscope—A Triple Operating Microscope. Plastic and Reconstructive Surgery. 1970 Mar 1;45(3):279-81;
2 O'Brien BM, Henderson PN, Crock GW. Metallized microsutures. Med J Aust. 1970 Apr 4;1(14):717-9. doi: 10.5694/j.1326-5377.1970.tb116874.x. PMID: 5427040
3 Henderson PN, O'Brien BM, Parel JM. An adjustable double microvascular clamp. Medical Journal of Australia. 1970 Apr;1(14):715-7; O'Brien BM.
4 O'Brien BM. A modified triploscope. Br J Plast Surg. 1973 Jul;26(3):301-3. doi: 10.1016/0007-1226(73)90020-9. PMID: 4726113.
5 O'Brien BM, Crock GW, Bennett RC, Henderson PN, Galbraith JE. Experimental and clinical microsurgery. Med J Aust. 1970 Apr 4;1(14):708-9. doi: 10.5694/j.1326-5377.1970.tb116871.x. PMID: 5427037
6 O'Brien BM, Henderson PN, Bennett KC, Crock GW. Microvascular surgical technique. Medical Journal of Australia. 1970 Apr;1(14):722-5
7 Baxter TJ, McC. O'Brien B, Henderson PN, Bennett RC. The histopathology of small vessels following microvascular repair. British journal of surgery. 1972 Aug;59(8):617-22
8 O'Brien BM, Miller GD, McLeod AM, Newing RK. Saving the amputated digit and hand. Medical Journal of Australia. 1973 Mar;1(11):558-62.
9 Taylor GI. Angiosomes Explored, Explained, Expanded and Explained. Chiron Journal of the University of Melbourne Medical Society. 1999 May 2;4(2):7-9.
10 Taylor GI, Daniel RK. The free flap: composite tissue transfer by vascular anastomosis. Aust. N. Z. J. Surg. 1973; 43: 1–3.
11 Daniel RK, Taylor GI. Distant transfer of an island flap by microvascular anastomoses. Plastic and reconstructive surgery. 1973 Aug 1;52(2):111-7.
12 O'Brien BM, MacLeod AM, Hayhurst JW, Morrison WA. Successful transfer of a large island flap from the groin to the foot by microvascular anastomoses. Plastic and Reconstructive Surgery. 1973 Sep 1;52(3):271-8.
13 Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. British journal of plastic surgery. 1987 Mar 1;40(2):113-41.
14 Taylor GI, Townsend P, Corlett R. Superiority of the deep circumflex iliac vessels as the supply for free groin flaps: clinical work. Plast Reconstr Surg. 1979 Dec;64(6):745–759
15 Taylor GI, Townsend P. Composite free flap and tendon transfer: an anatomical study and a clinical technique. Br J Plast Surg. 1979 Jul;43(4):170–183
16 Taylor GI, Miller GDH, Ham FJ. The Free Vascularised Bone Graft: A Clinical Extension of Microvascular Techniques. Plast Reconstr Surg 55(5):533-544, May 1975
17 Taylor GI, Townsend P, Corlett R. Superiority of the deep circumflex iliac vessels as the supply for free groin flaps: clinical work. Plast Reconstr Surg. 1979 Dec;64(6):745–759.
18 Conde JF, Quintero KV, Córdova LF, Haro CE, Dominguez JR. Angiosome Origins and Concept. International Journal of Medical Science and Clinical Research Studies. 2023 Dec 26;3(12):3208-10.
19 Rozen WM, Rajkomar AK, Anavekar NS, Ashton MW. Post-mastectomy breast reconstruction: a history in evolution. Clinical breast cancer. 2009 Aug 1;9(3):145-54.
20 Hamilton R, Fogdestam I. Australia’s contribution to the free abdominoplasty flap in breast reconstruction. Australasian Journal of Plastic Surgery. 2019 Dec 2;2(2):8-12.
21 Holmström H. The free abdominoplasty flap and its use in breast reconstruction: An experimental study and clinical case report. Scandinavian journal of plastic and reconstructive surgery. 1979 Jan 1;13(3):423-7.
22 Morrison WA, O'Brien BM, MacLeod AM. Thumb reconstruction with a free neurovascular wrap-around flap from the big toe. The Journal of Hand Surgery. 1980 Nov 1;5(6):575-83.
23 Adani R, Petrella G. Free “Wrap-Around” Great Toe Flap for Thumb Reconstruction After Avulsion Injuries. InClinical Scenarios in Reconstructive Microsurgery: Strategy and Operative Techniques 2022 Nov 27 (pp. 413-422). Cham: Springer International Publishing.
24 Lineaweaver W. The first free flaps and the problems they addressed. Annals of Plastic Surgery. 2014 Dec 1;73(6):623-4.
25 Australian Institute of Health and Welfare. Cancer data in Australia. Australian Institute of Health and Welfare; 2024. Accessed September 20, 2024. https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia
26 Cancer Australia. Influencing best practice in breast cancer. Cancer Australia; 2016. Accessed September 20, 2024. https://www.canceraustralia.gov.au/publications-and-resources/cancer-australia-publications/influencing-best-practice-breast-cancer
27 Dayaratna N, Nguyen CL, Spillane A, Mak C, Warrier SK, Dusseldorp JR. Trends and variations in post‐mastectomy breast reconstruction rates in Australia over 10 years. ANZ Journal of Surgery. 2023 Jan;93(1-2):242-50.